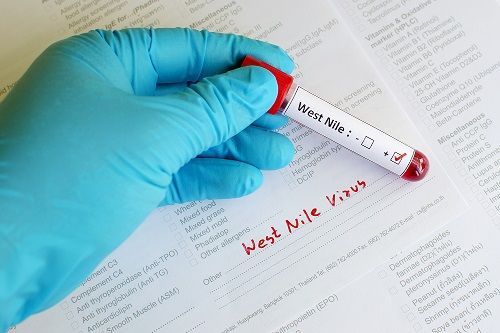
A Rare Case of Positive Heterophile Antibody in a Patient With West Nile Virus - Contagionlive.com
FINAL DIAGNOSIS
West Nile virus meningitis
HISTORY OF PRESENT ILLNESS
A 22-year-old woman presented to the emergency department in August with headache and dizziness lasting 2 days. Her headache was located on her left posterior head and was a sharp pain that radiated to her forehead. It eventually spread to both sides of her forehead and was throbbing in nature. She took ibuprofen without any relief. When her headache started, she also noticed dizziness that felt like the room was spinning and was triggered with movement of her head. This led to an episode of nausea and vomiting. A review of systems was also notable for photophobia, but negative for fever.
MEDICAL HISTORY
Class 3 obesity, asthma, migraines, acne vulgaris, chlamydia, gonorrhea
KEY MEDICATIONS
Ibuprofen 2 to 3 times a day for about 3 days
EPIDEMIOLOGICAL HISTORY
The patient was born in Pennsylvania and has not had any recent domestic or international travel. She is sexually active with men and had vaginal receptive intercourse without the use of a condom 2 weeks prior to presentation. She smokes marijuana occasionally, but denies any other illicit drug, alcohol, or tobacco use. She currently resides in a homeless shelter where she has seen mice but has had no known physical contact with them. She has had several mosquito bites over the past week. Her children recently had symptoms of an upper respiratory tract infection, and she has had no other known sick contacts. She is adopted and her biological sister has a history of systemic lupus erythematosus.
PHYSICAL EXAMINATION
The patient's vitals were notable for a fever of 102.4 °F, but she was otherwise hemodynamically stable and on room air. On examination, she was diaphoretic and had occasional rigors. She had no nuchal rigidity, but had dizziness with movement of her head. She had nontender cervical lymphadenopathy bilaterally. Her integumentary exam was notable for papules and pustules along her forehead, chin, and buttocks, and a single papule on her right thigh. Her neurologic exam revealed no focal deficits.
STUDIES
The patient's lab work was notable for a white blood cell count of 13 B/L (reference range, 4.0-11.0 B/L) with 87% neutrophils, hemoglobin level of 9.6 g/ dL (reference range, 12.5-15.0 g/dL), and mean corpuscular volume of 60 fL (reference range, 80-99 fL). The remainder of her complete blood count and comprehensive metabolic panel were within normal limits.
CLINICAL COURSE (SUMMARY OF HOSPITAL COURSE PRIOR TO DIAGNOSIS)
The woman presented to the emergency department and had a normal computerized tomography (CT) scan of her head. She was discharged with meclizine. However, her headache and severe vertigo persisted, and the next day she returned to the emergency department. She had a CT angiography of her head and neck, which showed normal vasculature but was notable for multiple, mildly enlarged cervical lymph nodes up to 1.5 cm. She received ketorolac (Toradol), metoclopramide, and diphenhydramine but her symptoms persisted, so she was admitted for intractable headaches.
Several hours after admission, she was noted to be febrile for the first time to 102 °F. Due to her fevers and headache, she was started on empiric acyclovir, vancomycin, ceftriaxone, and dexamethasone for meningitis. Magnetic resonance imaging of her brain was recommended by the neurology service but was unable to be obtained due to her class 3 obesity (body mass index, 62 kg/m).
A lumbar puncture was performed, with the results noted below. Due to her pustular rash on cheeks, chin, buttocks, and right thigh in the setting of fevers and cervical lymphadenopathy, and a new sexual partner 2 weeks prior, there was a concern for monkeypox. Monkeypox polymerase chain reaction (PCR) swabs were collected and ultimately ended up being negative. After she received an evaluation by the dermatology department, her pustular lesions were believed to be in line with her acne vulgaris as well as folliculitis.
DIAGNOSTIC PROCEDURES AND RESULTS
The patient's workup was negative for a fourth-generation HIV screen; treponemal antibody, Lyme serologies, QuantiFERON-TB Gold, blood cultures, urine gonorrhea, and chlamydia PCR also were negative. A heterophile antibody test was positive in the emergency department, but Epstein-Barr virus (EBV) serologies were consistent with past infection rather than acute infection (viral capsid antigen [VCA] IgG positive, VCA IgM negative, EBV nuclear antigen–positive), and cytomegalovirus (CMV) PCR from blood was negative.
A lumbar puncture showed an opening pressure of 33 cm H2 O (reference range, 5-25 cm H2 O); white blood cells, 285/ uL (reference range, 0-5 /uL), with 60% neutrophils, 30% lymphocytes, and 10% monocytes; glucose, 59 mg/dL (reference range 40-70 mg/dL); protein, 33 mg/dL (reference range, 15-45 mg/dL); and 60/ uL red blood cells (reference range, 0/uL).
A meningitis/encephalitis PCR panel was negative (including PCR for Haemophilus influenzae, Listeria monocytogenes, Neisseria meningitidis, Streptococcus agalactiae, Streptococcus pneumoniae, Escherichia coli K1, Cryptococcus neoformans/C gattii, herpes simplex virus (HSV)-1, HSV-2, varicella-zoster virus, human herpesvirus–6, CMV, enterovirus, and human parechovirus).
Cerebral spinal fluid (CSF) gram stain and bacterial culture were negative. Additional CSF studies were negative for HSV PCR, cryptococcal antigen, and lymphocytic choriomeningitis virus antibodies. Because of the patient's reports of mosquito bites, West Nile virus (WNV) serologies from her CSF were ordered; her WNV IgM was elevated above 5.00 (reference range, < 0.90), with WNV IgG negative. She was diagnosed with WNV meningitis and her antibiotics were discontinued.
TREATMENT AND FOLLOW-UP
For her WNV meningitis, the patient was treated with supportive care and defervesced on hospital day 3. For her vestibular neuritis secondary to her meningitis, she was started on scopolamine and meclizine with daily improvement in her symptoms. After approximately 14 days, her vertigo resolved.
DISCUSSION
Our case describes a young woman who presented with an acute onset of headaches and dizziness and was found to have aseptic meningitis. Through a detailed history, it was discovered that she had multiple mosquito bites over the preceding week, which prompted CSF testing for WNV serologies; this ultimately led to her diagnosis. The differential for aseptic meningitis is broad and includes, but is not limited to, WNV, lymphocytic choriomeningitis, Lyme disease, St Louis encephalitis virus, tuberculosis, HIV, HSV, syphilis, enteroviruses, Angiostrongylus cantonensis, leukemia, lymphoma, metastatic malignancies, certain autoimmune conditions, and medication induced (particularly trimethoprim-sulfamethoxazole and nonsteroidal anti-inflammatories).
During the evaluation of aseptic meningitis, a detailed epidemiologic history is vital to determine risk factors and narrow down the differential diagnosis. WNV is a ribonucleic acid virus under the genus Flavivirus. It is an arbovirus transmitted by the bite of infected mosquitoes, particularly Culex species. The virus is able to reach high levels in infected birds. Mosquitoes become infected when they feed on infected birds and they can then transmit the virus when they bite people or other animals.
The virus can also be transmitted through blood transfusion or organ transplantation.1 The majority of people infected with WNV (approximately 70%-80%) are asymptomatic. Those who do have symptoms often have nonspecific ones such as headaches, weakness, myalgias, or arthralgias. Up to 50% of patients may have a transient maculopapular rash. Less than 1% of those infected may develop neuroinvasive disease, which can manifest as meningitis, encephalitis, or acute flaccid paralysis.2
In one study with 16 serologically confirmed cases of West Nile neuroinvasive disease, 5 patients (31%) had meningitis, 8 (50%) had encephalitis, and 3 (19%) had poliomyelitis-like acute flaccid paralysis. Neuroinvasive symptoms such as meningitis, encephalitis, and flaccid paralysis may present separately or in conjunction.3
WNV infection should be suspected in patients who have been exposed to mosquitos with a febrile illness with or without acute neurologic deficit. In immunocompetent patients, diagnosis is made by finding positive IgM serologies in the serum or CSF. A PCR screen of serum or CSF can be obtained. However, the degree of viremia is often too low to be detected. The PCR screen may be positive if obtained early in the course of infection or in immunocompromised individuals who may have higher levels of viremia and a delayed IgM response.4
Although positive IgM antibodies to WNV are suggestive of recent WNV infection, there is cross-reactivity with other flaviviruses. The Centers for Disease Control and Prevention or state laboratories can run additional testing such as plaque reduction neutralization tests to rule out cross-reactivity and confirm the diagnosis.5
Early in this patient's diagnosis, a heterophile antibody was positive, initially raising concern for acute EBV. However, her EBV serologies were consistent with past infection. Although there have been no reported cases of positive heterophile antibody in patients with WNV in the literature, there is a case report of a false-positive heterophile antibody in a patient with dengue fever, which is in the Flavivirus genus with WNV.6
Treatment for WNV infection is supportive care. There have been case reports suggesting possible benefit from corticosteroids or intravenous immunoglobulin, although the data are conflicting; ultimately, supportive care is the standard treatment for WNV infections, including neuroinvasive disease.7 Those with neuroinvasive disease may have persistent symptoms for months to years after diagnosis.8
References
1. Bennett JE, Dolin R, Blaser MJ. Flaviviruses. In: Bennett JE, Dolin R, Blaser MJ. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020.
2. Zou S, Foster GA, Dodd RY, Petersen LR, Stramer SL. West Nile fever characteristics among viremic persons identified through blood donor screening. J Infect Dis. 2010;202(9):1354-1361. doi:10.1086/656602
3. Sejvar JJ, Haddad MB, Tierney BC, et al. Neurologic manifestations and outcome of West Nile virus infection. JAMA. 2003;290(4):511-515. Published correction appears in JAMA. 2003;290(10):1318.
4. Busch MP, Kleinman SH, Tobler LH, et al. Virus and antibody dynamics in acute West Nile virus infection. J Infect Dis. 2008;198(7):984-993. doi:10.1086/591467
5. West Nile virus: clinical evaluation & disease. Centers for Disease Control and Prevention. Updated July 7, 2021. Accessed October 5, 2022. https://www.cdc.gov/westnile/healthcareproviders/healthCareProviders-ClinLabEval.html.
6. Boyd K, Harrison JM, Kavanaugh MJ. False-positive monospot in a returning traveler with Dengue fever. Mil Med. 2018;183(3-4):e235-e236. doi:10.1093/milmed/usx046
7. West Nile virus: treatment & prevention. Centers for Disease Control and Prevention. Updated November 9, 2021. Accessed October 5, 2022. https://www.cdc.gov/westnile/healthcareproviders/healthCareProviders-TreatmentPrevention.html
8. Murray KO, Garcia MN, Rahbar MH, et al. Survival analysis, long-term outcomes, and percentage of recovery up to 8 years post-infection among the Houston West Nile virus cohort. PLoS One. 2014; 9(7):e102953.doi:10.1371/journal.pone.0102953
Comments
Post a Comment