“Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): a prospective, interventional, non-randomised, controlled study - The Lancet” plus 4 more
“Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): a prospective, interventional, non-randomised, controlled study - The Lancet” plus 4 more |
- Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): a prospective, interventional, non-randomised, controlled study - The Lancet
- Evaluation of the novel coronavirus disease in Turkish children: Preliminary outcomes - Wiley
- Coronavirus recovery: Most common post-COVID signs which could indicate signs of long term trouble - Times of India
- What you – and doctors – should watch for if you have COVID-19 - The Conversation US
- Coronavirus in San Diego and California: Latest updates and news - CBS News 8
| Posted: 08 Oct 2020 03:32 PM PDT [unable to retrieve full-text content]Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): a prospective, interventional, non-randomised, controlled study The Lancet | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Evaluation of the novel coronavirus disease in Turkish children: Preliminary outcomes - Wiley Posted: 29 Sep 2020 12:00 AM PDT 1 INTRODUCTIONCoronaviruses (CoVs) are RNA viruses that are related to human disease.1 The virus responsible for novel coronavirus disease (COVID‐19) is located in the same genus as the severe acute respiratory syndrome coronavirus (SARS‐CoV) and the Middle East respiratory syndrome coronavirus (MERS‐CoV). The new nomenclature of the virus has been accepted as severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2).2 Among the coronaviruses causing disease in humans, HCoV 229E, NL63, OC43, and HKU1 are the most frequently isolated ones. Despite the fact that all coronaviruses can infect subjects of all ages, these subtypes are responsible for endemics of upper respiratory tract infections in adults. However, many other coronavirus subtypes can also cause severe disease in humans.3-5 Coronaviruses are capable of undergoing mutations that lead to the emergence of novel CoVs that can be transmitted from animals to humans. SARS‐CoV was the first virus that was transmitted from bearcats to humans in 2002, resulting in the death of hundreds of people in 37 countries. After 10 years, in 2012, MERS‐CoV was first described in humans and caused 858 fatalities.6, 7 In December 2019, the novel SARS‐CoV‐2 was reported in Wuhan, China. After this date, the number of patients increased rapidly, and the disease became prevalent all over the world. A number of studies on the total burden of novel COVID‐19 have demonstrated that the disease is generally more dangerous in adults who are at risk of COVID‐19 related complications due to chronic underlying diseases such as cardiovascular and cerebrovascular diseases as well as diabetes.8 Otherwise COVID‐19 also commonly occurs in healthy children, a considerable proportion of whom experience severe disease leading to hospitalization, more frequent outpatient visits, prescription of pharmaceutical medications, and (although rarely) even death.9 The first‐ever pediatric COVID‐19 case in the world was reported from Shenzhen, China on January 20, 2020.10 Although several studies from Asia and America have reported that the new coronavirus disease may be less serious in children than adults,11, 12 subsequent studies from European countries have shown that the number of pediatric multisystem inflammatory syndrome cases related to COVID‐19 has increased over time; since then, case reports of the pediatric patients have been published from different regions of the world.13-15 The optimal management of the COVID‐19 disease is not clear and no treatment with proven reliability and effectiveness is yet available. Although there are several studies on possible drugs altering the prognosis of pediatric COVID‐19, there is no consensus for its treatment.16-22 The drugs already used for the treatment often cause adverse effects. To our knowledge, no major study has yet been published on pediatric COVID‐19 in Turkish children. Therefore, we aimed to evaluate the clinical, radiological, and laboratory features of the disease in Turkish children and to compare the data about disease characteristics with the data reported from other countries. In addition, this retrospective study also aimed to identify risk factors associated with COVID‐19 in Turkish children. 2 MATERIALS AND METHODSThis study included 105 patients aged 0–18 years, who were diagnosed with COVID‐19 at Dicle University Faculty of Medicine, Department of Pediatrics between April 2020 and June 2020. This department is the main tertiary center for the management of pediatric COVID‐19 patients in the southeastern region of Turkey. The diagnosis of COVID‐19 was made by real‐time reverse transcription‐polymerase chain reaction (RT‐PCR) studied from upper respiratory tract samples obtained via nasopharyngeal swabbing. Individuals who have had close contact with a person who has a confirmed or probable COVID‐19 infection without taking protective measures against droplet infection are tested in our hospital. In the first 3 months of the pandemic, very strict rules were implemented in our country. All adult and pediatric patients who were diagnosed with COVID‐19 were hospitalized, and after being followed up for the first few days, discharged home. Afterward, they were instructed to stay at home for 14 days and stay away from public areas. During the diagnostic procedures, BUN, creatinine, alanine aminotransferase (ALT), aspartate aminotransferase (AST), serum electrolytes, coagulation parameters, C‐reactive protein (CRP), procalcitonin, troponin I, CK‐MB, and d‐Dimer were studied in all patients. A posterior‐anterior (PA) chest radiogram was taken in every pediatric patient included in the study to determine whether the disease had lung involvement. Chest computed tomography (CT) was performed in cases of pathological findings on the radiogram or in clinically severe and critical cases. All data presented in the study related to biological tests and X‐Ray were obtained on the first day of hospital admission. The patients' demographic data, laboratory data, clinical data, and data on previous treatment approaches were accessed retrospectively from the patients' written medical records and computer‐based medical records. The severity of the disease was classified as asymptomatic, mild, moderate, severe, and critical according to the clinical characteristics, laboratory results, and chest radiography findings.23
The patients were divided into three age groups across which the study data were compared. These groups were as follows: Group 1, patients aged 0–1 year (0–12 months); Group 2, patients aged 1–10 years (13–120 months); Group 3, patients aged 10 to 18 years (130–216 months). Patients older than 18 years of age, those who had suspected COVID‐19 infection based on clinical, laboratory, and radiological findings but a negative RT‐PCR test result were excluded from the study. All patients and their legal guardians were informed in detail about the study protocol and provided written informed consent. The approval was taken from the Republic of Turkey Ministry of Health and Dicle University Faculty of Medicine local the Ethics Committee. 2.1 Statistical analysisData analyses were performed by using Statistical Package for Social Sciences (SPSS), Version 20.0 for Windows (SPSS Inc.). The variables were investigated using visual (histograms, probability plots) and analytical methods (Kolmogorov–Smirnov test) whether or not they were normally distributed. Normally distributed variables were shown by means and standard deviations, and non‐normally distributed variables were shown by median and range (maximum and minimum). The χ2 test was used to analyze categorical variables. Correlations between various parameters were studied using Pearson or Spearman correlations. Multiple groups were compared using a one‐way analysis of variance (ANOVA) with a posthoc Bonferroni correction and Kruskal–Wallis test for the normally and non‐normally distributed variables, respectively. The independent predictors of length of hospital stay were investigated by using stepwise multiple linear regression analysis. p values < .05 were considered statistically significant. 3 RESULTSThe mean age of the patients was 108.64 ± 65.61 months (1.5 months–18 years). Of the patients, 51.4% (54/105) were male. There were 13 patients in Group 1, 46 patients in Group 2, and 46 patients in Group 3. The most common route of COVID‐19 transmission in pediatric patients was a contact with a family member with COVID‐19 (n = 91, 86.7%). Four (3.8%) patients had an accompanying disease at the time of diagnosis. A 17‐year‐old patient had more than one comorbidity (Diabetes Mellitus + Beta thalassemia major + chronic respiratory disease). A 5.5‐month‐old patient was followed‐up for primary hemophagocytic lymphohistiocytosis before the diagnosis. A patient had Down syndrome and acute lymphoblastic leukemia, and another patient had epilepsy and was on antiepileptic drugs. The most common admission complaints were dry cough (n = 17, 16.2%), fever (n = 16, 15.2%), lassitude and fatigue (n = 14, 13.3%), and headache (n = 12, 11.4%). The admission complaints of the patients were summarized in Table 1.
Chest CT was performed in 48 patients. Pulmonary ground‐glass opacities (n = 11, 10.4%) were the most common chest CT finding. Other common findings were local patchy shadows (n = 5, 4.7%) and bilateral patchy shadows (n = 4, 3.8%), respectively (Figure 1). Pleural effusion was also seen in one of our patients.  (A) Bilateral ground glass and consolidation areas (black arrow) in a 7‐ month old girl with fever and cough,; (B) The CT image of a 9‐ month old girl with a history of fever, cough and close contact with a family member, revealing peripheral ground‐glass areas (black arrow) in both lungs; (C) Computed tomography (CT) of a A 17‐year‐old girl with dyspnea and cough revealing ground glass and peribronchial consolidation areas (White arrow) A significant number of patients were asymptomatic (n = 59, 56.2%). However, three patients required intensive care. The classification based on clinical severity was summarized in Table 1. The mean length of hospital stay was 4 (range 1–19) days for the patients who required hospitalization. No mortality was observed in any of our patients. Antibiotics and antiviral agents were used to treat the patients. The most commonly used drugs were the combinations of azithromycin (n = 72, 68.6%), hydroxychloroquine (n = 21, 20%), antibiotics (n = 10, 9.5%), oseltamivir (n = 8, 7.6%), and lopinavir‐ritonavir (n = 4, 3.8%). Only three patients required oxygen supplementation. High flow oxygen was administered to a patient who required intensive care. The clinical and laboratory findings of the patients were summarized in Table 2.
A comparison between Groups 1, 2, and 3 revealed that the rate of contact history was significantly lower in Group 1 than the other two groups (p < .001). The ratio of male gender was significantly higher in Group 2 (p = .032) than the other two groups. Sore throat and cough were significantly more frequent in Group 3 than the other two groups (p = .004, p = .008, respectively; Table 3).
The distribution of the clinical parameters according to disease severity was shown in Table 4. A comparison of clinical symptoms by gender revealed no statistically significant difference. A comparison of the laboratory parameters by gender revealed that the procalcitonin level was significantly higher in girls (0.227 ± 0.943) compared to boys (0.014 ± 0.05; p = .031).
The WBC and d‐dimer levels, lymphocyte, and platelet counts were significantly higher in Group 2 compared to the other two groups (p = 007, p = .05, p < .001, p < .001, respectively). The creatinine levels were lower in Group 1 than the other two groups (p < .001). Creatinine values are known to vary by muscle mass, so this finding was considered uninterpretable. The blood urea levels were lower in Group 1 than Group 3 (p = .048). The laboratory parameters that have shown significant differences across the study groups are summarized in Table 5.
The length of hospital stay was higher in patients who used chloroquine + Azithromycin + Oseltamivir and chloroquine + Azithromycin + oseltamivir + Lopinavir‐Ritonavir compared to those who did not receive any specific treatment (p = .012, p < .001, respectively). There were significant positive correlations between length of hospitalization and urea, CK‐MB, CRP, ferritin, fibrinogen, body temperature, heart rate; length of hospitalization showed negative correlations with oxygen saturation, hemoglobin level (p < .005). We performed a multiple linear regression analysis with the "enter" method to define the independent predictors of the length of hospital stay. Gender, CRP, ferritin levels, fibrinogen, and oxygen saturation were included in the analysis. CRP was the only independent factor associated with a longer duration of hospitalization (p < .001, Table 6).
4 DISCUSSIONAlthough many case series have been reported about COVID‐19 in children, the epidemiological and clinical patterns of COVID‐19 in pediatric patients remain largely unclear despite its rapid spread worldwide. This report aimed to evaluate the epidemiological characteristics, clinical findings, and treatment outcomes of COVID‐19 in pediatric patients in the southeastern region of Turkey. Children can carry the heaviest burden of viral respiratory diseases. However, corona‐ virus‐related infections also vary widely in severity among children. Studies from China and America have suggested that children with COVID‐19 might be less sick than adults and that pediatric cases might not describe various symptoms clearly as adults do.11, 12 Nevertheless, disease characteristics have not been described yet for pediatric patients from Turkey. This study aimed to determine the epidemiological characteristics of pediatric COVID‐19 patients from Turkey during the first 3 months (April–June 2020) of the disease. Our study included pediatric cases confirmed with a positive RT‐PCR test. The male/female ratio in COVID‐19 varies between studies. In earlier reports from China and the United States of America, boys outnumbered girls.11, 12, 16, 24 An American report provided data on signs and symptoms of COVID‐19 in 291 of 2,572 pediatric cases aged <18 years. A retrospective analysis of 115 children from China reported a male/female ratio of 1/0.58. The present study showed a male (51.4%) predominance, similar to what has been described in the Chinese and American populations.25-27 In earlier studies, patients' age ranged between 1 day and 18 years.11, 12, 25 In our study, the mean age of the patients was 108.64 ± 65.61 months, and the age range of them was 45 days–18 years. These results suggest that children of all ages are suspectible to COVID‐19. In a Chinese study, the most common symptoms in children with COVID‐19 were fever and dry cough (36%, 19%, respectively).25 Another previous large‐scale study also reported that fever and cough are more frequently observed in pediatric COVID‐19 cases (56%, 54%, respectively). In our study, the most common symptoms on admission were cough (16.2%), fever (15.2%), lassitude, and fatigue (13.3%). In an American study, the frequency of sore throat, headache, and diarrhea have been found to be quite lower in pediatric patients.12 The present study recorded various symptoms including sore throat, headache, diarrhea, loss of taste, anosmia, and vomiting (8%, 20%, 4%, 2%, 3%, and 6%, respectively). These findings are in line with other studies from other countries and suggest that children do not always have signs and symptoms such as fever and cough. Comorbidities were present in 3.8% of our patients and included diabetes mellitus, beta‐thalassemia major, chronic respiratory disease, Down syndrome, acute lymphoblastic leukemia, and epilepsy.28 However a study from the USA reported that the most common underlying conditions were chronic lung disease, cardiovascular disease, and immunosuppression. In a previous report on 2135 pediatric patients with COVID‐19, the disease followed asymptomatic, mild, moderate, severe, and critical courses. Regarding severity, 4.4%, 51.0%, and 38.7% cases were diagnosed as asymptomatic, mild, and moderate, respectively (total 94.1% of all cases).11 In another study, it was found that children with COVID‐19 had milder clinical manifestations, with nearly half of pediatric patients have been asymptomatic.25 In our study, 56.2% of the cases were asymptomatic; 30.5% were mild; 10.5% were moderate, and 2.9% were severe; none of our patients was in a critical condition. The percentage of patients requiring ICU admission was 2.9%. Laboratory findings in pediatric COVID‐19 patients are generally similar to those in other coronavirus infections. The number of white cells is often normal or low; neutropenia and/or lymphopenia may accompany COVID‐19. Thrombocytopenia may also develop. C reactive protein and procalcitonin levels are normal. In severe cases, liver enzymes and lactate dehydrogenase may increase, and abnormal coagulation and high d‐dimer levels have been reported in some cases.29 In our study, we found abnormal biological markers including elevated lactate dehydrogenase and elevated d‐dimer levels in three cases with severe disease. A 6‐month‐old male patient infected with COVID‐19 had high ferritin, d‐Dimer, LDH levels, and abnormal coagulation. A 17‐year‐old girl infected with COVID‐19 who had insulin‐dependent type one diabetes (HbA1C: 8.6), history of bone marrow transplant due to beta‐thalassemia major, and bronchiolitis obliterans had high ferritin, d‐Dimer, LDH, C‐reactive protein, and procalcitonin values. Thoracic tomography findings in children are bilateral, multiple, and patchy nodular ground‐glass opacities and/or infiltrations in the middle and peripheral zones of the lung or at the subpleural area. In the present study, pulmonary ground‐glass opacities (n = 11, 10.4%) were the most common finding in chest tomography. Other common findings included local patchy shadows (n = 5, 4.7%) and bilateral patchy shadows (n = 4, 3.8%). In one of our patients, pleural effusion was seen. These results are consistent with other reports.16, 24, 30 The radiological findings are nonspecific and milder than adults.22, 24, 30, 31 In a French study by Gaboriau et al., there were a total of 192 children with confirmed (n = 157) or highly suspected (n = 35) SARS‐CoV‐2 infection. Eighty‐five (44.3%) children had a normal chest X‐ray. CT was performed in 36 children and showed abnormalities in 26 (72.2%), including consolidations and/or ground‐glass opacities.32 To date, there are no published controlled clinical trials on specific drug therapies for pediatric COVID‐19 infection. As with other age groups, there is insufficient evidence for any drug that can be used in the treatment of COVID‐19 in children. Therefore, suggested treatments for COVID‐19 in children should be evaluated in accordance with the studies on adults. World Health Organization and the American Center for Disease Control and Prevention do not recommend specific drug treatment of children with COVID‐19.33, 34 The management of pediatric patients with COVID‐19 is also evaluated by the Scientific Board of Ministry of Health of Turkey at frequent intervals and revisions are made in Turkey.35, 36 Treatment strategies in this study were applied in accordance with the recommendations of the guidelines issued by the Republic of Turkey Ministry of Health. Probable adverse effects of drugs must be taken into consideration while making decisions for the treatment of pediatric patients. Treatment should be specifically assessed for each pediatric patient, with medication(s) being reserved for patients with probable severe pneumonia as well as for mild cases with risk factors. Drugs used in the treatment of our patients included azithromycin (n = 42, 40%), hydroxychloroquine (n = 21, 20%), empirical antibiotics (n = 10, 9.5%), oseltamivir (n = 8, 7.6%), lopinavir‐ritonavir (n = 4, 3.8%), and Favipiravir (n = 1, 0.9%). Only three patients needed supplemental oxygen therapy. High‐flow humidified oxygen was administered to a patient who was followed up at the intensive care unit. Long‐term studies are needed to find an effective treatment for children. There were some limitations to our study. First, this study was hospital‐based, second, the data may be incomplete and/or erroneous due to the retrospective study design. 5 CONCLUSIONTo our knowledge, this study is the largest cohort of pediatric patients with COVID‐19 reported from Turkey. A clear understanding of the local epidemiology of coronavirus infections and identification of risk factors is critical for the successful implementation of a prevention and control program. Longer term prospective studies are needed to provide a clear understanding of the local epidemiology of respiratory tract infections, to identify risk factors, to successfully implement a prevention and control program, and to clarify the role of respiratory pathogens. CONFLICT OF INTERESTSThe authors report that there are no conflict of interests. The authors alone are responsible for the content and writing of the paper.
REFERENCES
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Posted: 15 Oct 2020 06:43 AM PDT  For many COVID survivors, testing negative is only half the battle won. COVID-19, as an infectious viral disease induces a heavy burden on the body and can leave patients suffering from symptoms long after recovery, no matter how mild or severe the infection was. Latest findings from the National Institute of Health, Britain (NIH) suggest that infection possibilities not just multiply post-COVID, but can also launch a multi-pronged attack, causing possibly a 'rollercoaster' of symptoms affecting all parts of the body and mind. While doctors suggest that full recovery would require a month or two post-infection, SARS-COV-2 can also leave lasting consequences for the body's vital organs, and require acute health monitoring for a long time. From heart trouble, thrombosis to nervous disorders, there are some COVID signs which could indicate signs of long term trouble. Take a look: 02/6Heart damagePeople who have made successful recoveries from COVID are returning to hospitals complaining of discomfort, fullness and cardiac complications, despite having no pre-existing history for heart problems. Some have also been asked to go for preventive screenings in the long run. In fact, incidents of myocardial injuries and infraction are some of the most common post-COVID issues people face and leave lasting damage in the long run. According to doctors, the heart is one of the most vital organs impacted by COVID, and the implications can be harsh for everyone, no matter what age, severity, immunity or condition they have. At a preliminary level, it may lead to a decrease in heart function. This could be a result of either the systemic inflammatory response to infection or direct viral infection in the heart. Excessive pressure or stress put on the lungs or the heart can also result in myocarditis, which can lead to arrhythmia or even heart failure, in rare cases. Hence, it's important to look out for preventive signs, keep a check on essential vitals and take action accordingly. Making changes to your diet and lifestyle, as part of rehabilitative care should also be paid attention to in the long run. 03/6Lung fibrosisApart from the heart, one of the ways SARS-COV-2 virus implicates your body functioning is attacking the lungs and scarring the linings across the respiratory organs, leading to a build-up of a threatening condition, commonly known as fibrosis. COVID-19 is primarily a respiratory infection and reduces vital functioning. Due to avid viral multiplication and compromised immune response, the virus can start to 'clot' parts of your respiratory system and make normal functions, such as breathing difficult for some. It is for the same reason, many experience bouts of breathlessness, fatigue, low oxygen saturation weeks or months after testing negative. All of these are some of the early signs of lung fibrosis and require acute care and support. Failure to take care at the earliest can have potentially faltering consequences for a person's health, especially for someone who is over the age of 50, or is prone to respiratory disorders. 04/6ThrombosisThrombosis refers to the formation of blood clots in the blood vessels, which prohibits proper blood flow through the body's circulatory system. In some cases, a reduced, or compromised blood flow could lead to an increased risk of some patients developing blood clots in the veins that cause leg clots (deep vein thrombosis) and pulmonary embolism. Experts say COVID-19, of all diseases, carries the most risk for increased rates of thrombosis for patients who are infected by it, as well as those who have tested negative. This is far more damaging for someone who is immuno-compromised or is suffering from diabetes. It is for the same reason that patients diagnosed with COVID and those who have pre-existing medical issues are advised to take blood thinners like aspirin on a prophylactic basis to cut down on chances of complications. 05/6Renal damageStudies emerging out of New York have detailed that intensive cases of COVID-19 caused long-term damage to the kidneys, with over 60% of critically ill COVID patients requiring support in the long term. Not only is this finding unexpected, but researchers also say that it is also one of the most 'silent' signs of degradation in the body. Problems like chronic kidney disease (CKD), renal failure are also being commonly reported amongst patients who have recovered from COVID-19. 06/6Cognitive decline and brain fogBrain fog, anxiety, depression, PTSD and a decreased quality of life are some of the symptoms COVID long haulers are talking about. It is just another way how a simple 'respiratory' virus could pose long term trouble for your brain and nervous system. Though it isn't entirely clear as to how and why does the COVID causing virus to impact your brain functioning, effects on your mental health could have lasting problems, and further slow down recovery. Cured patients are also reporting symptoms of memory loss, confusion, forgetfulness, likening them to dementia-like symptoms. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| What you – and doctors – should watch for if you have COVID-19 - The Conversation US Posted: 09 Oct 2020 05:29 AM PDT Even though President Donald Trump is back at the White House following his hospitalization for COVID-19, people around the world are watching his health, in addition to that of a number of other politicians who have tested positive for the disease. Infectious disease specialist and physician Kartikeya Cherabuddi, who has treated COVID-19 patients, explains what medical doctors monitor and how they treat patients, from the early days after an infection and the critical days that follow. Early symptoms and when to seek medical helpCommon early symptoms include those of the upper respiratory tract – sore throat, runny nose, cough – as well musculoskeletal symptoms, such as as muscle aches, joint pain and fatigue, as well as vomiting and additionally the loss of smell or taste. Fever is present in only a few patients. Many patients may have very mild or no symptoms. As the illness progresses, doctors monitor the lungs for symptoms, such as shortness of breath, or other organ-related problems, such as chest pain of cardiac origin. They sometimes observe confusion, extreme fatigue and weakness in the elderly. Difficulty breathing or the sensation of being out of breath, new confusion or the inability to stay awake, chest pressure or pain are reasons for being evaluated and for possible hospitalization. Monitoring body temperature is not as helpful for evaluating whether one needs to be hospitalized but a pulse oximeter, which measures your blood oxygen level, can be quite helpful. The higher your risk for severe disease, the lower the threshold should be for being evaluated. In addition to knowing symptoms, it's a good idea to have a COVID-19 plan for all members of your family. Here's how to start:
Watching for a second wave after the first weekSymptoms may worsen initially as they progress from the upper respiratory tract to the lungs. A second wave of worsening symptoms can then happen after the first week (often day 8 to 10) of illness, when the immune response goes into overdrive. 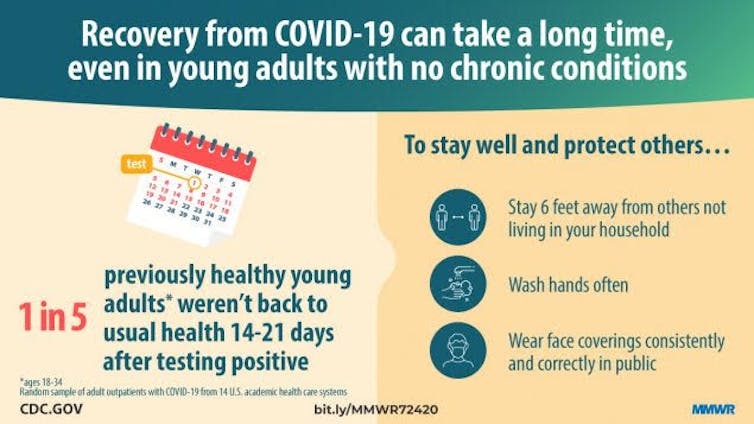 In high-risk individuals, it is important during this period after the first week to monitor the patient and to avoid a false sense of security. Worsening shortness of breath, rapid breathing, the use of additional muscles to breathe, difficulty in getting sufficient oxygen and the appearance of being unwell are some of the signs practitioners watch for. A breathing rate above 30-per-minute or a low oxygen level with a new requirement for supplemental oxygen is classified as severe COVID-19. Why the immune system response is criticalDuring early onset of infection, a person's immune system kicks in with a broad, nonspecific response to the virus, which is especially effective in kids. Immune system proteins called interferons appear to control the infection. The immune cells that attack seasonal coronaviruses which cause common colds do not appear to control the infection but may limit disease severity, duration or both. From days 5 to 14 after infection, a person's adaptive immunity, which is specific and targeted to SARS-COV-2, takes over. It involves three components - antibodies, killer and helper T-cells. This response needs to be coordinated and controlled. This is often not the case in the elderly, and could explain the more severe illness that is seen in older individuals. Antibodies can eliminate, or neutralize, the virus. These immune cells and their products - cytokines, interleukins and interferons – can control infection but in severe cases go out of control. This produces a severe imbalance and causes the cytokine "storm" in adults or the multisystem inflammatory syndrome in children. Doctors carefully follow the patient's symptoms, exam findings and clinical and laboratory parameters, such as blood tests that measure levels of specific proteins to determine if the patient's immune system is over-reacting. Critical illness due to COVID-19 develops in 5% of all patients but occurs in 1 in 5 individuals requiring hospitalization.  Levels of treatment – mild to severeFor people who test positive for COVID-19 but are asymptomatic or have mild symptoms, there is no proven, effective therapy. Getting a good night's sleep and exercise and limiting anxiety are helpful. It is recommended that you maintain physical separation but stay in touch with family or friends. Taking vitamin D could provide some benefit, and has been shown in one metanalysis of studies to protect against acute respiratory infections. Those with very low vitamin D levels benefited the most. For people with mild to moderate symptoms, monitoring for any symptoms or signs of worsening in addition to pulse oximeter readings is recommended. Blood oxygen levels should be 94% or over in those with no underlying lung disease. If able, you can walk a little and repeat pulse oximetry, gradually increasing to 6 minutes of walking. For people with severe disease who are hospitalized, there are a number of therapies available:
Lingering effects and 'long haulers'Doctors have known that viral infections, including measles, can cause long-term symptoms. Forty percent of survivors of severe acute respiratory syndrome, or SARS, which was also caused by a coronavirus, have reported having residual effects even 3.5 years later. Persistent symptoms for COVID-19 sufferers, termed "long haulers," sometimes occur even in young adults and children with no underlying medical conditions. In a telephone survey of symptomatic adults who were never hospitalized, 1 in 3 people overall and 1 in 5 among those aged 18 to 34 had not returned to their usual health 14 to 21 days after testing. Symptoms that persist include fatigue, cough, shortness of breath, loss of taste or smell, headache and body aches. Individuals with severe illness requiring hospitalization may take up to six weeks to recover. Blood clots in the lung, brain and other areas have been reported but with a wide variable range of estimates. Sicker patients and those with more underlying risk factors have a higher incidence. These blood clots – in addition to viral and immune damage to the lungs, heart and brain – can lead to prolonged ill health, decreased mobility and mental issues. A practical and useful guide to rehabilitation self-management after COVID-19 related illness is available from the World Health Organization. [Get facts about coronavirus and the latest research. Sign up for The Conversation's newsletter.] Long-term mental effects are an area of tremendous concern. Doctor offices should perform follow-up phone calls, establish post-COVID-19 clinics, and make mental health resources available. Patients and family members can monitor breathing, exercise tolerance, swelling of limbs, body weight and mental activity, and be on the lookout for signs of depression. For an individual patient, the course of illness and complications both immediate and long-term are unpredictable. They need to be closely monitored for two weeks following diagnosis for the second wave of worsening and for up to six weeks for recovery if hospitalized with severe illness. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Coronavirus in San Diego and California: Latest updates and news - CBS News 8 Posted: 13 Oct 2020 03:14 PM PDT  Real-time updates and developments around the coronavirus outbreak and how it is affecting San Diego as we work to separate facts from fear. SAN DIEGO COUNTY, Calif. — Key COVID-19 facts in San Diego and California:
Oct. 15
City parking enforcement to resume in San Diego ThursdayFollowing a two-week warning period, the City of San Diego will resume parking regulation enforcement across the city Thursday after months of limited enforcement due to the COVID-19 pandemic. According to the city, restarting parking enforcement will allow for increased turnover at parking meters and businesses, ensuring accessibility for patrons visiting local stores and restaurants.
Oct. 14
Beyond the Numbers: San Diego County to submit health equity plan to the stateSan Diego County will submit its health equity plan to the state Thursday, which could eventually help reduce the county's case rate. The newly developed metric is aimed at giving counties credit toward its rate for undertaking initiatives in historically underserved communities where coronavirus has hit hardest. The equity metric reviews the percentage of positive cases in communities that make up a county's lowest quartile under the California Healthy Places Index. The index is developed by reviewing 25 indicators, including economic, education and environment factors in different communities. In San Diego, it includes portions of the South Bay, El Cajon, Oceanside, Escondido and East County.
San Diego County remains in red tier, but warns against complacencySan Diego County reported 303 new COVID-19 cases and four new deaths on Wednesday. This means 844 people have died from COVID-19 countywide. On Wednesday, the county stressed that people receive a flu shot to keep people out of hospitals this winter. You can watch the county's full update here.
Oct. 13
San Diego County reports 14 new COVID-19 deaths on TuesdaySan Diego County will remain in the red, or substantial, tier of the state's four-tier COVID-19 reopening plan for at least another week, even as public health officials reported 278 new COVID-19 infections and 14 deaths from the illness. According to the California Department of Public Health, San Diego County's state-calculated, adjusted case rate is 6.8 daily infections per 100,000 residents, up from 6.5 the previous week. The unadjusted case rate was 7.2, up from 6.9 last Tuesday. The adjusted rate is due to San Diego County's high volume of tests, but still leaves the county on the precipice of the state's most restrictive tier -- purple. The testing positivity percentage is 3%, below last week's 3.5%, and is in the third -- or orange -- tier. To remain in the second tier of the four-tier COVID-19 reopening plan, the county must continue to have an adjusted case rate of less than 7.0 per 100,000 residents and a testing positivity percentage of less than 5%. The new cases and deaths reported Tuesday raised the total for the region to 51,024 cases and 840 deaths. Eight women and six men died between Oct. 3 and Sunday. Their ages ranged from the early 50s to early 100s. All but one had underlying medical conditions.
San Diego County remains in red tier with 6.8 adjusted case rateSan Diego County avoided being pushed back into the state's most restrictive purple tier Tuesday and will remain in the second -- or red -- tier of the state's four tier COVID-19 reopening plan at 6.8 adjusted case rate per 100,000 residents and a testing positivity percentage of 3.4%, according to data from the state.
UC San Diego partners with National City on COVID-19 vaccine trialUC San Diego has partnered with National City on a COVID-19 vaccine trial. Mayor Alejandra Sotelo-Solis and the city council unanimously voted in support of hosting one COVID-19 vaccine trial location in National City to strengthen vaccine trial access for the South Bay region. View all News 8 coverage of coronavirus / COVID-19
BACKGROUND:On February 11, 2020 the World Health Organization announced an official name for the disease that is causing the 2019 novel coronavirus outbreak, first identified in Wuhan China. The new name of this disease is coronavirus disease 2019, abbreviated as COVID-19. In COVID-19, "CO" stands for "corona," "VI" for "virus," and "D" for disease. Formerly, this disease was referred to as "2019 novel coronavirus" or "2019-nCoV". There are many types of human coronaviruses including some that commonly cause mild upper-respiratory tract illnesses. COVID-19 is a new disease, caused by a novel (or new) coronavirus that has not previously been seen in humans. Currently, there is no vaccine, however, the CDC suggests the following precautions, as with any other respiratory illness:
Know how it spreads:
Protect yourself and others
Wash your hands often
Avoid close contact
Cover your mouth and nose with a cloth face cover when around others
Cover coughs and sneezes
Clean and disinfect
Monitor your health daily
The California Department of Public Health has issued guidance on the use of cloth face coverings to protect against the spread of the novel coronavirus COVID-19. As of April 4, 2020, all employees in San Diego County who may have contact with the public in any grocery store, pharmacy/drug store, restaurant or food establishments, convenience store or gas station are required to wear a cloth face covering while at work as an additional measure to help "flatten the curve" in the San Diego region. As of May 1, San Diego County requires everyone in the county to wear face coverings in many public settings. The coverings help prevent the spread of COVID-19 and are part of our path to reopening San Diego. See full health order here. While officials say these face coverings are not a substitute for practices like social distancing and handwashing, there is evidence to suggest that the use of cloth face coverings by the public during a pandemic could help reduce disease transmission. Officials do not recommend the public use N-95 or surgical masks which are needed by health care workers and first responders. |
| You are subscribed to email updates from "respiratory system disorders,respiratory system facts,respiratory tract infection" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment