The comparative study of chronically ill and healthy children and adolescents in the light of their general mental health ... - Nature.com
Abstract
Children's hospitalisation is difficult for the family and the immediate environment. In these cases, the provision of psychological support is particularly important. Chronically ill children who are regularly hospitalised are in a particularly difficult situation, often feeling vulnerable. Our research aims to explore and analyse in detail the psychological state, attitudes and mental health of chronically ill children and to compare patient groups (children receiving care in pulmonology, gastroenterology, onco-haematology and rehabilitation) to understand the interacting factors, which may be of great importance for quality patient care and for measures to improve patient care in the future. We studied chronically ill children (N = 107) aged 10 to 18 years (M = 14.3; SD = 2.0), cared for by the Department of Paediatric Rehabilitation, Paediatric Psychiatry and Psychosomatics of the University of Debrecen Clinical Centre, the second largest paediatric institution in Hungary. In our survey, sociodemographic questions, the Connor–Davidson Resilience Scale, the Satisfaction With Life Scale, the Cantril Ladder, the Non-Productive Thoughts Questionnaire, the Problematic Internet Use Questionnaire, the Drawing version of Pictorial Representation of Illness Self-Measure (PRISM-D), the Beck Depression Inventory—Shortened Scale, the Illness Intrusiveness Ratings Scale, the Spielberger State-Trait Anxiety Questionnaire—Child Version and the Strength and Difficulty Questionnaire were applied. One-way analysis of variance (ANOVA) was used to examine differences between groups, and Pearson rank correlation analysis was used to measure the relationships between individual variables. The results show significant differences between patient groups in terms of resilience, depression, nonproductive thoughts, problematic internet use, anxiety and coping, but no consistent pattern in the development of scores. In addition, for some psychological correlates, the role of sociodemographic background also showed significant results. The practical utility of our study is that using questionnaire methods to map patient satisfaction, compliance, and patient attitudes will provide regarding the factors that influence the mental health status of children living with chronic illnesses. In the light of this, additional methods and tools can be included to improve the quality of healthcare and to develop a set of procedures that will serve the intended purpose.
Similar content being viewed by others

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial

Delirium
Introduction
Chronic diseases permanently change the way we live and require constant adaptation. Chronicity is characterised by an unpredictable course of illness, reduced physical performance/ability, changes in physical appearance, persistent dependence on specialists, treatment, technical aids and physical assistance, and changes in life prospects1, and therefore the impact of chronic illness on personality and psychological well-being is significant, providing a good basis for the relevance of research in this area.
Chronic disease management requires a long-term care plan, and treatment adherence is paramount to achieving better health outcomes, quality of life and cost-effective health care2. The World Health Organization's guideline on adherence behaviour states that "increasing adherence may have a greater impact on health than improving specific medical therapy"3. However, chronic disease and its treatments place broad behavioural demands on adolescents. Precisely scheduled daily medication, consumption of special dietary products, regular exercise, regular visits to health care providers and monitoring blood glucose levels are just some of the demands. Asthma attacks and other attacks, periods of intense pain, immobility and unpredictable situations can aggravate their condition. These needs affect almost every aspect of adolescents' lives, including school, eating, sports, work and travel. Self-care problems are, therefore, common among children and adolescents with chronic illnesses. Non-cooperation with the doctor and non-adherence to recommendations and instructions is a major problem. Previous studies have shown that about 50% of chronically ill adolescents do not adhere to care recommendations, but this has a significant impact on health4. In the United States, it is estimated to cause about 125,000 deaths, at least 10% of hospitalisations, and a significant increase in morbidity and mortality2.
Recent literature on medical communication and disease behaviour has consistently distinguished between disease process and disease representation, whereby disease process refers to the phenomena that can be detected by physical examination with instruments, and disease state refers to how the patient represents the disease in his or her cognition. The clinician and the treatment team must gather sufficient information about both to ensure the effectiveness of treatment5, which can also provide an adequate physical and psychological basis for self-management of the disease. The importance of understanding and promoting self-management in the care of chronic diseases in children is becoming increasingly evident, not only through research and clinical efforts but also through the introduction of new health policies. However, this is not so simple, as self-management is a complex phenomenon determined by the influence of several factors, both separately and in combination. The theory of Modi et al.6 provides an excellent illustration of self-management. Self-management comprises three interdependent parts: self-management behaviours, contextual variables in four domains (individual, family, health system, community influences) that affect implementing these behaviours, and processes that link influences to self-management behaviours. Thus, compliance, adherence and self-management are not measured and examined in isolation but in context.
Our study aims to map children's and adolescents' sociodemographic characteristics, their reactive behaviour, subjective somatic health complaints, health status, illness representation, life satisfaction, vision, presence of non-productive thoughts, problematic internet use and illness burden. Our research started in 2021 at the Department of Paediatric Rehabilitation, Psychology and Psychosomatics, University of Debrecen, University of Debrecen. During the research, we set two research questions:
- 1.
Is there a difference in the development of mental health indicators in the patient groups?
- 2.
Can any differences in the mental health-related variables alongside the sociodemographic background variables?
- 3.
Is there a correlation between the different mental health indicators?
Based on the research questions, we formulated the following hypotheses:
H1: Significant differences can be experienced regarding the mental health status (resilience, coping, satisfaction with life, future, anxiety, non-productive thoughts, problematic internet use, depression, and illness representation) between the healthy and chronically ill children; we hypothesise that children living with chronic illnesses report worse mental health status.
H2: Significant differences can be found in the mental health status of children regarding the sociodemographic background variables; girls, children whose parents have lower educational attainment and those who received their diagnosis in a later life stage can be experienced with worse mental health status.
H3: We hypothesise that positive mental health-related variables (resilience, coping, satisfaction with life, future) are in positive relationship with the other positive mental health-related variables and are in negative connection with negative variables (anxiety, non-productive thoughts, problematic internet use, depression, and illness representation).
Psychological characteristics of children with chronic illness
Children with chronic illnesses frequently manifest non-productive thoughts, reflecting the intricate interplay between their health challenges and cognitive processes7. These non-productive thoughts often encompass heightened health-related anxiety, fear of stigmatization, and concerns about missed academic or social opportunities8. Research underscores the impact of these cognitive patterns on mental health outcomes and overall well-being. Interventions targeting cognitive restructuring and fostering adaptive coping mechanisms become pivotal in mitigating the detrimental effects of non-productive thoughts9.
The prevalence of anxiety and depressive symptoms among children with chronic illnesses is a well-documented concern in the realm of pediatric healthcare. Extensive research consistently reveals heightened rates of depression in this population, attributable to the prolonged nature of their health challenges and associated psychosocial stressors10,11. Elevated symptomatology often compromises the quality of life and adherence to medical regimens, necessitating targeted interventions12,13. Recognition of the widespread nature of depressive symptoms in children with chronic illnesses underscores the urgency for integrated mental health support within healthcare frameworks14. A comprehensive approach is indispensable, aiming to alleviate the burden of depression and enhance the overall well-being of these vulnerable individuals.
The relevance of addictions, particularly problematic internet use, among children with chronic illnesses is a critical facet requiring scholarly attention. These vulnerable individuals may turn to excessive online engagement as a coping mechanism, potentially exacerbating mental health challenges15. Addressing this intersection demands a nuanced understanding of the intricate relationship between chronic illness and addictive behaviours. The issue of problematic internet use encompasses individuals who excessively devote their time to online activities, disregarding their other daily responsibilities. This behavior ultimately leads to negative effects on both their physical and psychological health. Fluctuations in academic performance, disruptions in sleep and nutrition, social isolation, and involvement in risky behaviors linked to substance abuse are all correlated with problematic internet use16,17.
Resilience and coping holds profound relevance among children grappling with chronic illnesses, serving as a crucial determinant of their adaptive capacity and overall well-being18. Extensive empirical evidence highlights resilience as a multifaceted construct, encompassing psychological, social, and cognitive dimensions19. Understanding and fostering resilience in this population prove essential, as it mitigates the adverse psychological impact of chronic illnesses, facilitates effective coping strategies, and enhances overall quality of life20,21. Moreover, resilient children exhibit a greater capacity to navigate healthcare complexities, adhere to treatment regimens, and sustain positive social relationships.
The role of sociodemographic background variables in the development of mental health indicators
The impact of sociodemographic background on the psychological characteristics of children grappling with chronic illnesses is a multifaceted domain warranting comprehensive examination. Socioeconomic status significantly influences access to healthcare resources, shaping the child's psychological resilience and coping strategies22. Economic disparities may contribute to heightened stress, impacting mental well-being23. Cultural influences play a pivotal role in shaping the perception of illness, attitudes toward treatment, and the utilization of support networks24. Family dynamics, influenced by sociodemographic factors, contribute to the child's psychosocial environment, affecting emotional regulation and adaptive coping25. Moreover, geographic location and community resources further shape the psychological landscape of these children. Rural and urban disparities may result in differential access to specialized healthcare services and support systems26. Educational opportunities and social integration, influenced by sociodemographic factors, are integral components impacting psychological development.
The sociodemographic background of children facing chronic illnesses holds profound relevance in understanding variations in resilience and coping mechanisms. Factors such as socioeconomic status, cultural influences, and familial support significantly impact how children navigate persistent health challenges27. Socioeconomic disparities may shape access to resources and support networks, influencing resilience levels28. Recognizing the nuanced interplay between sociodemographic factors, resilience, and coping is imperative for healthcare providers, educators, and policymakers. Tailored interventions must consider these variables, ensuring equitable support for children across diverse sociodemographic backgrounds as they confront the intricate complexities of chronic illnesses.
Methods
Sample
Our study included children aged 10–18 years with a chronic disease who regularly attend the Paediatric Clinic's gastroenterology, pulmonology, onco-haematology and paediatric rehabilitation departments and one of their parents/guardians. The questionnaires were administered in the personal presence of the PhD student conducting the research, each time under the supervision of the clinical psychologist professor conducting the research. Respondents were asked to complete the questionnaire on a voluntary basis. In all cases, intellectual disability and illiteracy were excluded from the study. The assumption that a 10-year-old child is able to complete a test package of this structure and length independently was also an important factor in the selection of the age group.
During the research, convenience sampling method was used to gather participants for a questionnaire survey, where they completed several questionnaires. The inclusion criteria of the research group were the presence of any chronic disorder, being under medical treatment in the Paediatric Clinic's of the University of Debrecen Clinical Centre and being less than 18 years old. The control group consisted of the peers of such children (below 18 years) not having any chronic disorder and not being under medical treatment. Having any kind of chronical illness was considered as exclusion criteria regarding the control group and being older than 18 years for both groups.
The total research sample consists of children and caregivers (294 children and one parent per child), of whom 107 chronically ill children and parents had their questionnaires analysed while they were complete. Among the parents and children, some decided not to continue participating in the study during the test administration: 53 cases occurred, the reasons being difficulties in completing the test, tiredness, train departure, etc. It is also worth mentioning that the pandemic period of COVID-19 caused by the SARS-CoV-2 virus, a pandemic infectious disease, also made it difficult to take the test on several occasions when people preferred to spend the minimum time in and around the clinics. Once they had undergone the necessary medical examination, they tried to leave as soon as possible. Overall, the total number of children considered for this current research was N = 207 (see further details in Table 1).
Instruments
With children and adolescents, we took a pre-assembled set of tests to assess the components of the personality profile of children with chronic illnesses that might be related to our study objective in the reviewed literature.
Sociodemographic questionnaire
We formulated questions regarding gender, age, type of settlement, highest educational level of parents, family structure, subjectively assessed financial status, number of siblings, exact description of chronic disease(s), and achievement of independent (without the parent) sleep.
Connor–Davidson resilience scale 29
The questionnaire measures successful coping with stress, or the ability to recover from challenging circumstances. The person evaluates the statements related to of resilience on a 5-point Likert scale through a factor, scoring between 10 and 40 points (Cronbach's α = 0.851).
Satisfaction with life scale 30
This test consists of a 5-item scale that assesses one's overall cognitive evaluation of life satisfaction, rather than measuring positive or negative emotions. Participants express their level of agreement or disagreement with each item on a 7-point scale, ranging from strongly agree to strongly disagree (Cronbach's α = 0.74).
Cantril ladder 31
The Cantril Ladder serves as a visual tool for evaluating overall contentment and happiness in life. Individuals are shown an image of a ladder with numbers ranging from zero to ten. This scale represents the spectrum of life satisfaction, with zero representing the lowest level and ten representing the highest. Participants are then asked to consider their current life situation and position themselves on the ladder accordingly. If their score falls at or below four, it indicates a state of 'suffering', while a score of seven or higher signifies 'thriving'. Essentially, a higher score on the ladder corresponds to a greater sense of well-being and satisfaction with life (Cronbach's α = 0.86).
Non-productive thoughts questionnaire (NPT) 32
This is a single-factor scale for measuring ruminations and rumination in childhood, with scores ranging from 10 to 30. The scale uses 10 items to measure perseverative trait-like thoughts in the questionnaire. Participants were instructed to rate each item on a 3-point scale, with 1 indicating "not true," 2 indicating "sometimes true," and 3 indicating "often true." The scores on this scale reflected the frequency of nonproductive thoughts, with higher scores indicating a higher frequency (Cronbach's alpha = 0.84).
Problematic internet use questionnaire (PIU-Q) 33
The questionnaire uses a five-point scale to assess the level of agreement with the provided statement. The obsession subscale delves into contemplation and fantasies revolving around the Internet, as well as the mental symptoms experienced when deprived of Internet access. The neglect subscale pertains to the disregard for daily tasks and fundamental necessities. Lastly, the control disorder subscale encompasses items that address challenges in regulating Internet usage (Cronbach's alpha = 0.84).
Drawing version of pictorial representation of illness self-measure (PRISM-D) 34,35
Participants in the PRISM-D drawing test are provided with an A4-size sheet of paper containing a 7 cm yellow circle positioned in the lower right corner. This circle serves as a representation of the individual's self, mirroring the original PRISM test. Four subscales of the drawing test developed by the Hungarian working group of the PRISM test were considered: the distance between the yellow circle symbolising self and the circle symbolising illness, the average area of the circle representing illness (25.12 cm2), the number of circles representing youth resources, and the total area of the circles representing resources were compared.
The Beck depression inventory—shortened scale (BDI—R, shortened version) 36,37
Depression severity was assessed using the BDI, a questionnaire consisting of 21 items. These questions capture emotions experienced over a recent period of time. Each statement is assigned a score from 0 to 3, resulting in a total score that can range from 0 to 84 (Cronbach's alpha = 0.82).
The illness intrusiveness ratings scale (IIRS) 38
The IIRS is a concise tool that individuals can use to report their own experiences.
Originally designed to assist individuals dealing with chronic and potentially life-threatening illnesses, the IIRS can also be utilized by those with less severe health conditions. Consisting of 13 questions, this assessment prompts participants to evaluate the extent to which their illness and/or its treatment disrupt various aspects of their life that are crucial to overall quality of life.
To assess the level of intrusion caused by illness, participants utilize a seven-point scale that spans from 1 (minimal) to 7 (significant) (Cronbach's alpha = 0.86).
The Spielberger state-trait anxiety questionnaire : child version (STAI-S-C and STAI-T-C, state-trait anxiety inventory for children, STAI-C) 39,40
The STAI test was developed based on the adult questionnaire of the same name to assess anxiety levels in school-age children. The STAI-T is a scale that evaluates an individual's overall emotional state, while the STAI-S measures their current anxiety level specifically related to a particular event. Both scales consist of 20 items, with response options ranging from 1 (not experiencing at all) to 4 (experiencing intensely) (Cronbach's alpha = 0.77).
The strength and difficulty questionnaire (SDQ) 41,42
The questionnaire is designed to measure children's behavioural characteristics and abilities, and it shows a consistent picture compared to the parent version. It is a concise survey designed to evaluate behavioural patterns in individuals aged 2–17. The SDQ questionnaire inquires about a total of 25 characteristics, encompassing both negative and positive attributes. These characteristics are distributed across 5 subscales, each consisting of 5 items. The subscales measure emotional symptoms, conduct problems, hyperactivity, peer problems, and prosocial behaviour. The scores from the items in the first 4 subscales are combined to calculate a total difficulties score (Cronbach's alpha = 0.75).
Statistical analysis
A cross-sectional study was performed with a matched control group. Descriptive statistics were generated from the questionnaire data. The descriptive statistics are graphical representations of the scale of each variable to characterise and visualise the distributions, both for the population as a whole and for each of the diseases studied. One-way analysis of variance (ANOVA) was used to examine differences between groups, and Pearson rank correlation analysis was used to measure the relationships between individual variables.
Ethical approval and consent to participate
This research was conducted in accordance with the Declaration of Helsinki. The Institutional Research Ethics Committee—University of Debrecen Clinical Centre (REC—IKEB) approved this study (DE RKEB/IKEB 5858-2021). The research is conducted ethically, the results are reported honestly, the submitted work is original and not (self-) plagiarised, and authorship reflects the individuals' contributions. Informed consent was obtained from all subjects and/or their legal guardian(s).
Results
Sociodemographic characteristics of children
Overall, 107 children completed our questionnaire, with 58 boys (54.2%) and 49 girls (45.8%) in gender distribution. The mean age was 14.3 years (SD = 2.0). 48 (44.86%) live in county capitals, 12 (11.21%) in big cities, 28 (26.17%) in small towns and 19 (17.76%) in villages. This proportion can be considered ideal, as it was very important to us not only to get the opinion of the population living in the county town. Regarding birth order, one child has no siblings, 63 are first born, 26 are second born, and the remaining 17 are the third or later child in the family (Table 1).
83.8% of the respondents live with their parents, 9.1% with their mother, 3% with their father, 1% with a grandparent and 3% with a foster parent. 80.8% have a room of their own, and 19.2% do not have an own room at the moment. 78.8% sleep in their room, 11.1% share a room with their parents and 10.1% with their siblings. According to their subjective assessment of their financial situation, 84% say they live on a medium income, 13% on a low income, and 3% say they have a high income.
The distribution of patients was as follows: 34 (16.4%) from gastroenterology, 21 (10.1%) from onco-haematology, 19 (9.3%) from pulmonology and 33 (15.9%) from rehabilitation. 82 persons (76.64%) stated that there were no family members with a chronic disease among their immediate relatives. In comparison, 25 persons (23.36%) stated that there were children and/or adults with a chronic disease among their family members.
There is a significant difference in the distribution of the groups of ill and healthy children in terms of the mother's education (p = 0.001): mothers with tertiary education are over-represented in the group of healthy children, while mothers with a maximum of primary education are over-represented in the group of sick children. A similar trend is also observed for the educational attainment of fathers, although in this case, the difference in the distribution of the groups is not significant (p = 0.252).
Psychological characteristics of children
First, we tested H1 in which we supposed that children living with chronic illnesses report worse mental health status. The mean score for the whole sample regarding resilience was 28.26 (Fig. 1). Significant differences were found when comparing the groups (p = 0.040; η = 0.167; η2 = 0.028), with high scores for pulmonary and gastroenterological diseases. At the same time, below-average scores were also found for patients requiring rehabilitation, onco-haematological patients and healthy children. Patients requiring rehabilitation also show no difference in resilience levels compared to healthy children. They have coping resilience levels comparable to those of healthy children.
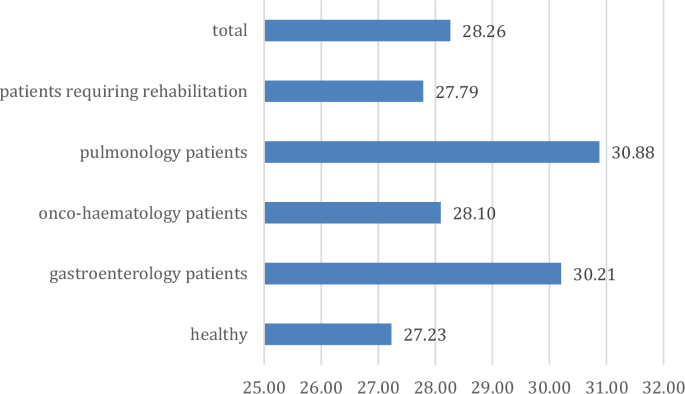
Distribution of resilience in the groups (points).
For Non-productive thoughts, the sample average is 20.22 points (Fig. 2). Compared to this mean, onco-haematological patients and healthy children showed higher scores. In contrast, children requiring rehabilitation diagnosed with pulmonary and gastrointestinal diseases showed lower scores, and although the difference is not significant, there is a trend level difference (p = 0.073; η = 0.189; η2 = 0.036).
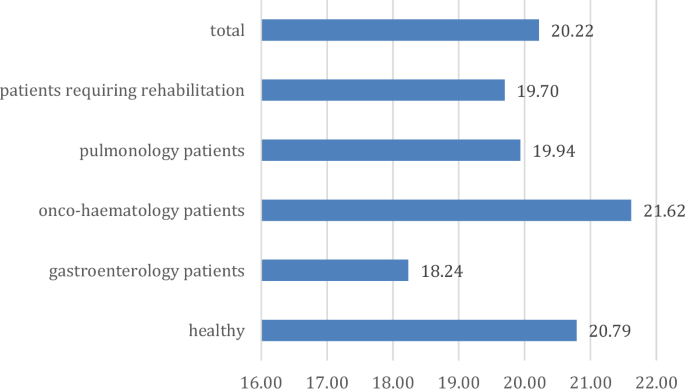
Non-productive thoughts scale scores across groups (points).
For Problematic internet use, the overall sample scores for preoccupation with the Internet (obsession) were 3.28, neglect of daily activities (neglect) was 5.25, and difficulty controlling internet use (control) was 4.07. The scores are increasing, with neglect being the most significant phenomenon (Table 2). For obsession, there is a significant difference between groups (p = 0.001; η = 0.146; η2 = 0.021), with above-average scores for onco-haematology and pulmonology patients. In contrast, gastroenterology patients have the lowest and below-average scores for children requiring rehabilitation and healthy children. A trend level difference was found for the control dimension (p = 0.072; η = 0.143; η2 = 0.120) with the same pattern. For the dimension of neglect, the difference between groups was insignificant (p = 0.253; η = 0.193; η2 = 0.027).
The four main variables of the PRISM-D test were examined (Table 3). The average distance between the yellow circle representing self and the circle representing disease was 11.32 cm in the sample. In this case, there is a significant difference between groups. Significantly lower values were observed for onco-haematology and pulmonology, while significantly higher values were observed for gastroenterology (p = 0.036; η = 0.251; η2 = 0.063). The average number of circles representing the resources of young people was 3.34, with a significant difference between groups (p < 0.001; η = 0.469; η2 = 0.220), with a similar pattern to the previous one. The average area of the circle representing illness is 25.12 cm2, which is significant compared to the area of the circle representing self, 38.47 cm2. No significant differences are observed in this respect (p = 0.526; η = 0.158; η2 = 0.025). The overall area of the circles representing resources is 104.91 cm2. There is no significant difference for the circle representing self (p = 0.526; η = 0.212; η2 = 0.045), although above-average values are also observed for patients requiring rehabilitation, pulmonology and gastroenterology. For the area of the circles representing resources, there are also strikingly low values for onco-haematology, pulmonology and patients requiring rehabilitation, but the difference is not significant (p = 0.169).
For the Beck Depression Questionnaire, a mean of 4.54 points was found for the whole sample. The difference between the groups is at a trend level (p = 0.073; η = 0.221; η2 = 0.049), with the highest scores in pulmonology and haematology patients and healthy subjects and the lowest in patients requiring rehabilitation and gastroenterology patients (Fig. 3).
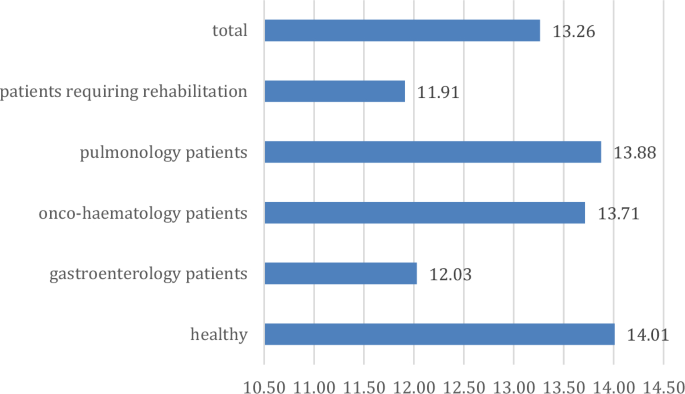
Trends in depression scores across groups (points).
On the STAI scale of state anxiety to performance anxiety, a score of 45.51 was available, and the trait anxiety level was 32.29, according to children's self-report (Table 4). There was no significant difference between groups in scores on the STAI scale of situational anxiety—performance anxiety (p = 0.614; η = 0.132; η2 = 0.018), with scores above average for patients requiring rehabilitation and onco-hematologcal treatment, close to average for healthy children and below average for gastroenterology and pulmonology patients. The scores on the STAI general anxiety scale showed trend differences (p = 0.064; η = 0.221; η2 = 0.051), with the highest scores in healthy children and the lowest scores in patients with gastroenterology and those requiring rehabilitation.
The scores on the Strength and Difficulties Questionnaire scales were as follows: 4.55 points on the Hyperactivity Scale, 2.95 points on the Emotional Symptoms scale, 2.15 points on the Behavioural Problems scale, 4.67 points on the Peer Problems scale and 7.75 points on the Prosocial scale. Only the Emotional Symptoms scale showed a trend difference (p = 0.075; η = 0.220; η2 = 0.048), with higher scores for onco-hematology and pulmonology patients and lower scores for gastroenterology patients (Table 5).
The role of sociodemographic background variables in the development of mental health indicators
Next, we tested H2, in which we supposed significant differences in the mental health status of children regarding the sociodemographic background variables. Thus, we examined which sociodemographic background variables play a significant role in the psychological variables. Significant and trend-level differences are presented along the trend of the results. Comparisons made to examine gender differences also highlighted some significant differences. For the Non-productive Thoughts Scale, higher scores for girls are seen (p = 0.025; η = 0.223; η2 = 0.049), as is the same trend for trait anxiety (p = 0.001; η = 0.312; η2 = 0.097), depression (p = 0.006; η = 0.218; η2 = 0.048) and emotional functioning (SDQ, p = 0.001; η = 0.196; η2 = 0.038). Further disease group-specific differences are not significant, presumably due to the rather small sample size (Fig. 4).
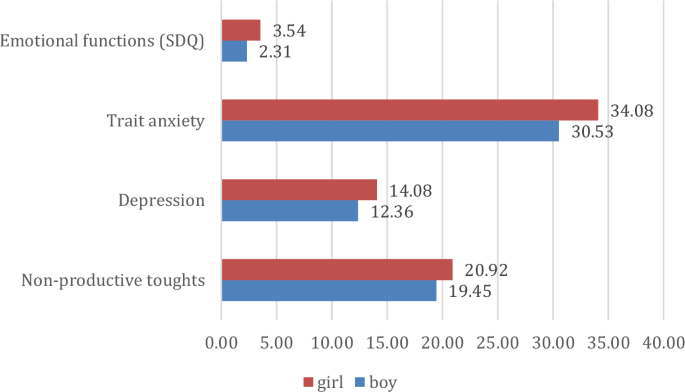
Major gender differences in mental health indicators (points).
We then examined the role of parental education on each mental health indicator (Fig. 5). Overall, a significant difference was found for resilience (maternal education: p = 0.006; η = 0.286; η2 = 0.082 paternal education: p = 0.011; η = 0.235; η2 = 0.055), which indicates that children of parents with low education have higher resilience scores. In addition, significant differences were found for the disease burden (mother's education: p < 0.001; η η = 0.26...
Comments
Post a Comment