Epstein–Barr virus-associated infectious mononucleosis with acute ... - BMC Infectious Diseases
A healthy 23-year-old male developed a 39 ºC fever with nausea and sore throat nine days before hospitalization. Seven days prior to hospitalization, the patient was examined at Clinic A, diagnosed with viral upper respiratory tract inflammation, and prescribed loxoprofen. Subsequently, he developed general malaise, nausea, and reduced appetite and visited Clinic B three days before hospitalization. Left cervical lymphadenopathy and liver inflammation (as evidenced by elevated aspartate aminotransferase and alanine aminotransferase levels) were observed, and IM was suspected. The patient was thus prescribed acetaminophen and referred to our facility two days before hospitalization. The patient had not recently traveled abroad and only had sexual intercourse with his partner. The patient presented with a headache, nausea, fever, sore throat, and joint pain; runny nose, nasal congestion, cough, abdominal pain, diarrhea, difficulty urinating, and feeling of residual urine were not observed.
The patient's state of consciousness was clear. His vital signs were as follows: blood pressure, 120/66 mmHg; pulse, 88 beats/min (regular); body temperature, 38.3 °C; respiratory rate, 18 breaths/min; and percutaneous oxygen saturation, 100% (indoor air). There was no extraoral tonsil enlargement. Bilateral posterior to anterior cervical lymphadenopathy was observed. The lymph nodes were soft and mobile, with no tenderness. Other superficial lymph nodes and hepatosplenomegaly were palpable. The Traube's space, which is defined by the area delineated by the left sixth rib superiorly, the left-mid axillary line laterally, and the left costal margin inferiorly, produced a tympanic sound.
Blood test results were as follows: white blood cell, 5000/µL; neutrophils, 66.5%, lymphocytes, 22.3%; monocytes, 10.5% atypical lymphocytes, 3.0%; aspartate aminotransferase, 112 U/L; alanine aminotransferase, 125 U/L; lactate dehydrogenase, 89 U/L; and C-reactive protein, 6.2 mg/dL.
Simple computed tomography of the chest, abdomen, and pelvis showed splenomegaly with a major axis of 11.5 cm. No hepatomegaly and mediastinal or intra-abdominal lymph node swelling was found.
Fever, tonsillar pharyngitis, lymphadenopathy, atypical lymphocytes in the peripheral blood, liver dysfunction, and splenomegaly were observed, and the patient was diagnosed with IM. Antibody titers of the viruses that can cause IM-like symptoms were assessed, and we followed up with the patient. The next day, the patient developed left testicular pain and was transferred to the emergency outpatient clinic for hospitalization. Pain, redness, and swelling were observed in the left scrotum. Physical examination revealed that lifting of the left testicle relieved the pain (positive Prehn's sign), suggesting epididymitis and excluding testicular torsion. Test results for the presence of leukocytes, bacteria, and gonococcal/chlamydia DNA by PCR in the urine were all negative, as were results for urine culture. Ultrasonography revealed swelling of the epididymis and increased blood flow, and the area was tender when palpated (Fig. 1). Testicular swelling or attenuated echo levels were not observed. The patient was hospitalized for left epididymitis.
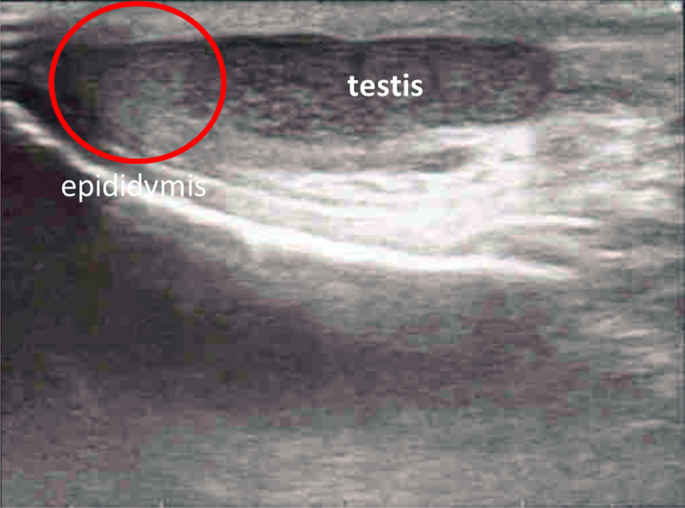
Ultrasonography of the left scrotum. No varicocele, hernia, or testicular torsion was observed. Left epididymis was swollen (red circle)
Because the patient presented with typical IM, it was likely that the cause was viral. Additionally, as the epididymitis was unilateral, this diagnosis would not affect fertility. Thus, we did not administer antibiotics; instead, the patient's genitals were iced, and acetaminophen was administered for symptomatic treatment. The patient's progress after hospitalization is shown in Fig. 2. Testicular pain, which scored 8 based on the Numerical Rating Scale at admission, slowly improved and decreased to 0 by day 11 of hospitalization. Furthermore, although the fever and liver dysfunction peaked on day 5, they slowly improved after that. On day 8, a rash without pruritus was observed on the patient's trunk and upper limbs, which also spontaneously improved. The patient continued to be hospitalized due to concerns on pain relapse and the development of new symptoms. Subsequently, acetaminophen treatment was discontinued, and no new symptoms appeared at least 5 days. After confirming that the pain was completely relieved, the patient was finally discharged on day 16.
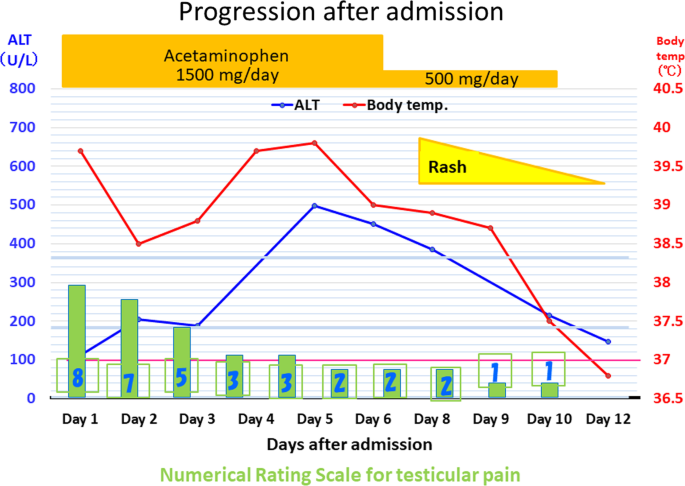
Disease progression in our patient after admission. The patient was not treated with antibiotics for disease but received acetaminophen for the symptomatic treatment of testicular pain. On days 5 and 6 after admission, the patient's ALT level and fever reached their peak but improved thereafter. On day 8, a rash without pruritus was observed on the patient's trunk and upper limbs and subsided by day 12, as did the patient's testicular pain. Finally, the patient was discharged on day 16. ALT alanine aminotransferase
The patient underwent tests for other potential pathogens, and the results were as follows: T-SPOT Mycobacterium tuberculosis, negative; human herpesvirus 6 IgM, < 10 (standard value: < 10), human herpesvirus 6 IgG, 30.5 (standard value: < 10), cytomegalovirus IgM, 0.7 (0–0.7), cytomegalovirus IgG, 12.3 (0–1.0), EBV early antigen IgM, 5.2 (< 0.5), EBV capsid antigen IgM, 3.2 (< 0.5); EBV capsid antigen IgG, 0.4 (< 0.5), Epstein–Barr nuclear antigen IgG, 0.3 (< 0.5), mumps IgM, 0.44 (< 0.8), mumps IgG, 7.6 (< 2.0), herpes simplex IgM, 0.4 (0–0.8), herpes simplex IgG, < 2.0 (< 2.0), and human immunodeficiency virus antigen/antibody, negative.
Table 1 shows the time course of the antibody titer of EBV. Changes in the antibody titer established a definitive diagnosis of IM caused by EBV. Based on the patient's progress, we diagnosed him with IM-associated unilateral epididymitis.
At present, 5 years have passed since the patient visited the hospital; to date, he has not experienced a recurrence of epididymitis. The patient got married and had children, and we have confirmed that fertility was not affected.
Comments
Post a Comment