“Human to animal transmission of SARS-CoV-2 in households is common - News-Medical.Net” plus 2 more
“Human to animal transmission of SARS-CoV-2 in households is common - News-Medical.Net” plus 2 more |
- Human to animal transmission of SARS-CoV-2 in households is common - News-Medical.Net
- The pressure is on for Australia to accept the coronavirus really can spread in the air we breathe - The Conversation AU
- Did COVID-19 Really Escape From A Lab? The Evidence Suggests It Did - MacIverInstitute
| Human to animal transmission of SARS-CoV-2 in households is common - News-Medical.Net Posted: 29 Apr 2021 12:00 AM PDT Coronaviruses are seen in multiple mammalian species. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of the COVID-19 pandemic, is said to have passed to humans from a mammalian source and to have originated from an animal reservoir as a zoonotic pathogen. Although the virus is spreading from person to person currently, the angiotensin-converting enzyme 2 (ACE2) receptor that facilitates the entry of SARS-CoV-2 is present in many species. There are several reports of domestic animals infected with SARS-CoV-2, including cats and dogs. So far, roughly 76 cats and 51 dogs have been reported to have confirmed SARS-CoV-2 infection by the USDA-APHIS based on antibody or PCR testing. Workplace SARS-CoV-2 transmission from humans to animals has been documented in zoos and on mink farms. This is in line with previous reports of cats and ferrets infected with SARS-CoV-1 and lab studies showing experimental SARS-CoV-2 infection in non-human primates, hamsters, rabbits, and ferrets. However, not much is known about the frequency and risk factors for SARS-CoV-2 transmission from humans to animals in a household setting. Community-based study of household pets to assess human to animal SARS-CoV-2 transmissionResearchers from the US recently carried out a community-based study of household pets with one or more confirmed SARS-CoV-2 cases in humans living in the household. Data was collected with the help of a survey of human and animal demographics and clinical parameters, human-animal contact, aspects in their shared environment. Blood was collected from the animals to test for anti-SARS-CoV-2 antibodies, and nasopharyngeal swabs were collected for PCR testing for the virus. The study is published on the bioRxiv* preprint server. 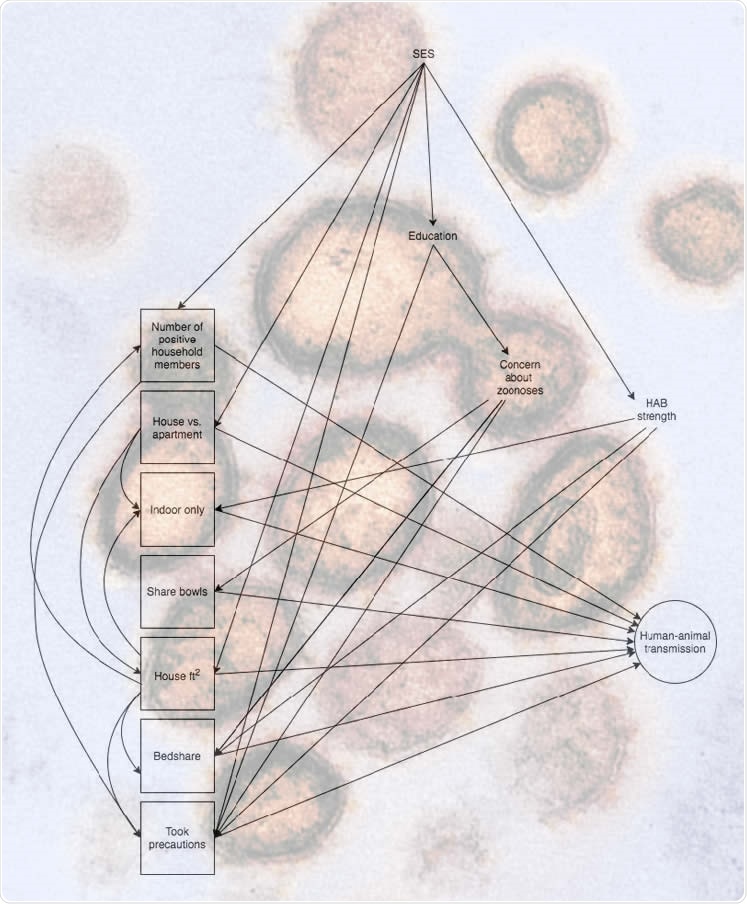 Directed acyclic graph for human-animal SARS CoV2 transmission. Variables outlined with a square are the exposures of interest, while outcome (approximated by serostatus, PCR result, and COVID-19 like illness in separate models) is outlined with a circle. HAB: human-animal bond; SES: socioeconomic status; took precautions: SARS-CoV-2 positive household member(s) took precautions to prevent transmission to pet; indoor-only: animal does not go outdoors; bedshare: animal shares a bed with one or more household members. 23.7% of the dogs studied had clinical symptoms of COVID-19 and 43.1% had SARS-CoV-2 antibodiesThe researchers have reported interim findings from their sampling of dogs. Samples were gathered from 67 dogs in 46 households. Results from nasopharyngeal testing were available for 58 dogs, and serological testing results for 51 dogs. Clinical symptoms of COVID-19 were reported in 14 dogs (23.7%), and SARS-CoV-2 antibodies were detected in 22 dogs (43.1%). The results of all PCR tests on nasopharyngeal swabs were negative. Survey results showed that close human-animal contact was common, and most households were aware of and followed measures to minimize human-to-animal transmission of SARS-CoV-2 after diagnosis. Although there were no statistically significant associations between human-animal contact variables and COVID-19-like illness or seropositivity in dogs, there were positive trends for sharing beds with humans and the number of virus-positive humans in the corresponding household. Measures reportedly taken to mitigate transmission to pets showed a protective trend. A dog with a COVID-19-like illness was also found to be seropositive for the virus.
Findings show that human-to-animal SARS-CoV-2 transmission in households is quite commonThe findings indicate that the transmission of SARS-CoV-2 from human-to-animal in households is common in a study population with close human-animal contact. They also show that infected pets often show signs of COVID-like disease. Although nasopharyngeal sampling of dogs did not show positive PCR results in this study, it could be because of delays in sampling. Household members were taking precautions to protect companion animals from SARS-CoV-2 infection, which indicated an opportunity for implementing more measures to decrease transmission of SARS-CoV-2 between humans and animals sharing households. According to the authors, the study offers important and novel insights into the cross-species transmission of SARS-CoV-2 in a household setting. Moreover, human, animal, and environmental data collected during the study represents an accurate One Health approach to this research. The findings indicate the willingness of households in the study population to adopt strategies to protect their pets from SARS-CoV-2 infection. These measures can effectively prevent household transmission of zoonoses and anthropozoonoses.
*Important NoticebioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information. Journal references:
|
| Posted: 12 May 2021 01:03 PM PDT More than a year into the pandemic, the World Health Organization (WHO) and US Centers for Disease Control finally changed their guidance to acknowledge SARS-CoV-2, the virus that causes COVID-19, can be transmitted through the air we breathe. In Australia, we've just had the latest leak from hotel quarantine, this time in South Australia. Investigations are under way to find out whether a man may have caught the virus from someone in the hotel room next to his, before travelling to Victoria, and whether airborne transmission played a role. These examples are further fuelling calls for Australia to officially recognise the role of airborne transmission of SARS-CoV-2. Such recognition would have widespread implications for how health-care workers are protected, how hotel quarantine is managed, not to mention public health advice more broadly. Indeed, we're waiting to hear whether official Australian guidelines will acknowledge the latest evidence on airborne transmission, and amend its advice about how best to protect front-line workers. The evidence has changed and so must our adviceAt the beginning of the pandemic, in the absence of any scientific studies, the WHO said the virus was spread by "large droplets" and promoted handwashing. Authorities around the world even discouraged us from wearing masks. A false narrative dominated public discussion for over a year. This resulted in hygiene theatre — scrubbing of hands and surfaces for little gain — while the pandemic wreaked mass destruction on the world. But handwashing did not mitigate the most catastrophic pandemic of our lifetime. And the airborne deniers have continually shifted the goalposts of the burden of proof of airborne spread as the evidence has accrued. Read more: Catching COVID from surfaces is very unlikely. So perhaps we can ease up on the disinfecting What does the evidence say?SARS-CoV-2 is a respiratory virus that multiplies in the respiratory tract. So it is spread by the respiratory route — via breathing, speaking, singing, coughing or sneezing. Two other coronaviruses — the ones that cause MERS (Middle Eastern respiratory sydrome) and SARS (severe acute respiratory syndrome) — are also spread this way. Both are accepted as being airborne. In fact, experimental studies show SARS-CoV-2 is as airborne as these other coronaviruses, if not more so, and can be found in the air 16 hours after being aerosolised. Several hospital studies have also found viable virus in the air on a COVID-19 ward. Established criteria for whether a pathogen is airborne scores SARS-CoV-2 highly for airborne spread, in the same range as tuberculosis, which is universally accepted as airborne. A group of experts has also recently outlined the top ten reasons why SARS-CoV-2 is airborne. So why has airborne denialism persisted for so long?The role of airborne transmission has been denied for so long partly because expert groups that advise government have not included engineers, aerosol scientists, occupational hygienists and multidisciplinary environmental health experts. Partly it is because the role of airborne transmission for other respiratory viruses has been denied for decades, accompanied by a long history of denial of adequate respiratory protection for health workers. For example, during the SARS outbreak in Canada in 2003, denial of protection against airborne spread for health workers in Toronto resulted in a fatal outbreak. Even influenza is airborne, but this has been denied by infection control committees. What's the difference between aerosols and droplets?The distinction between aerosols and droplets is largely artificial and driven by infection control dogma, not science. This dogma says large droplets (defined by WHO as larger than 5 micrometres across) settle to the ground and are emitted within 2 metres of an infected person. Meanwhile, fine particles under 5 micrometres across can become airborne and exist further away. There is in fact no scientific basis for this belief. Most studies that looked at how far large droplets travelled found the horizontal distance is greater than 2 metres. And the size threshold that dictates whether droplets fall or float is actually 100 micrometres, not 5 micrometres. In other words, larger droplets travel further than what we've been led to believe. Leading aerosol scientists explain the historical basis of these false beliefs, which go back nearly a century. And in further evidence the droplet theory is false, we showed that even for infections believed to be spread by droplets, a N95 respirator protects better than a surgical mask. In fact airborne precautions are needed for most respiratory infections. Why does this difference matter?Accepting how SARS-CoV-2 spreads means we can better prevent transmission and protect people, using the right types of masks and better ventilation. Breathing and speaking generate aerosols. So an infected person in a closed indoor space without good ventilation will generate an accumulation of aerosols over time, just like cigarette smoke accumulates. A church outbreak in Australia saw spread indoors up to 15 metres from the sick person, without any close contact. Masks work, both by preventing sick people from emitting infected aerosols, and by preventing well people from getting infected. A study in Hong Kong found most transmission occurred when masks weren't worn inside, such as at home and in restaurants. Read more: This video shows just how easily COVID-19 could spread when people sing together Coughing generates more aerosolsThe old dogma of droplet infection includes a belief that only "aerosol generating procedures" — such as inserting a tube into someone's throat and windpipe to help them breathe — pose a risk of airborne transmission. But research shows a coughing patient generates more aerosols than one of these procedures. Yet we do not provide health workers treating coughing COVID-19 patients with N95 respirators under current guidelines. At the Royal Melbourne Hospital, where many health worker infections occurred in 2020, understanding airflow in the COVID ward helped explain how health workers got infected. Think about it. Airborne deniers tell us infection occurs after a ballistic strike by a single large droplet hitting the eye, nose or mouth. The statistical probability of this is much lower than simply breathing in accumulated, contaminated air. The ballistic strike theory has driven an industry in plastic barriers and face shields, which offer no protection against airborne spread. In Switzerland, only hospitality workers using just a face shield got infected and those wearing masks were protected. Read more: Many of our buildings are poorly ventilated, and that adds to COVID risks In hotel quarantine, denial of airborne transmission stops us from fixing repeated breaches, which are likely due to airborne transmission. We need to select quarantine venues based on adequacy of ventilation, test ventilation and mitigate areas of poor ventilation. Opening a window, drawing in fresh air or using air purifiers dramatically reduce virus in the air. We need to provide N95 respirators to health, aged-care and quarantine workers who are at risk of high-dose exposure, and not place them in poorly ventilated areas. It's time to accept the evidence and tighten protection accordingly, to keep Australia safe from SARS-CoV-2 and more dangerous variants of concern, some of which are vaccine resistant. |
| Did COVID-19 Really Escape From A Lab? The Evidence Suggests It Did - MacIverInstitute Posted: 12 May 2021 05:29 AM PDT  Photo credit: Tom WolfDan O'Donnell tests Congressman Mike Gallagher's theory that COVID-19 was born in a lab and finds some surprising evidence.May 12, 2021 Guest perspective by Dan O'Donnell Wisconsin Congressman Mike Gallagher isn't one for conspiracy theories. As a U.S. Marine Corps intelligence officer, he was trained to deal only in facts. And now the facts are leading him unmistakably to a conclusion that for more than a year has been dismissed as crackpottery. COVID-19, he is convinced, escaped from a lab. "Flash back about a year ago and change, when there were a few of us who were suggesting that it was a remarkable coincidence that there was the [biosafety] level-4 biosafety lab located where this whole outbreak started," he said. This lab also just happened to be the epicenter of the entire nation's study of bat viruses. It is the home of Dr. Shi Zhengli, known as China's "Bat Lady" because of her research into bat-borne illnesses such as the SARS-CoV-1 virus that caused Asia's deadly SARS outbreak in 2002. Although the Chinese government has sealed her files, it was known that she had collected bats from the Yunnan province that carry the closest known relative of SARS-CoV-2. This is significant, because Yunnan is 1,000 miles away from Wuhan, making it all but impossible for a bat in the wild in Yunnan to infect a human in Wuhan and start a pandemic there. Early theories about the virus jumping to humans after an unlucky person ate a bowl of bat soup in the Huanan Seafood Wholesale Market in Wuhan were dismissed last May, effectively ruling out the market as the source of the outbreak. Moreover, bats hibernate in the winter months when the virus was supposedly first detected, so a human encounter with a wild bat was always a rather unlikely cause. "In order to prove the wet market theory, you have to prove that the host species somehow traveled 1,000 miles but didn't start an outbreak along the way," Gallagher explained, adding that a far more probable origin was a virus that had escaped during "gain-of-function" research at the Wuhan Institute of Virology. Gain-of-function is a type of medical experimentation in which viruses are induced to mutate into more transmissible and more dangerous versions. The goal is to study these mutations in order to better prepare humanity for the next deadly pandemic. Dr. Zhengling's work, for instance, was focused on mutating the SARS-CoV-1 virus so as to prevent another deadly SARS outbreak. This, Gallagher admits, is where things start to get a little crazy, especially since that research just might have been funded by a grant from the United States. Specifically the National Institutes of Health. Specifically the National Institute of Allergy and Infectious Diseases (NIAID). Specifically its director, Dr. Anthony Fauci. Gallagher does not suggest that Dr. Fauci and the Chinese government were conspiring to unleash a weaponized virus on the world, but rather that American researchers—who were prevented from doing gain-of-function research under a 2014 Obama Administration dictate—outsourced the work to the Chinese. In 2011, Dr. Fauci co-wrote a Washington Post op-ed entitled "A Flu Virus Risk Worth Taking," in which he argued that "important information and insights can come from generating a potentially dangerous virus in the laboratory." In other words, a decade ago he strongly supported gain-of-function research. "Understanding the biology of influenza virus transmission has implications for outbreak prediction, prevention and treatment," he wrote. "In defining the mutations required for mammalian transmission, public health officials are provided with genetic signatures that, like fingerprints, could help scientists more readily identify newly emergent, potentially harmful viruses, track their spread and detect threatening outbreaks. "The ability to identify such viruses even a few months faster than by conventional surveillance provides critical time to slow or stop an outbreak." In 2014, however, President Obama's White House put a three-year moratorium on gain-of-function research into SARS, MERS, and influenza viruses. That same year, Dr. Fauci's NIAID awarded a $3.4 million grant to EcoHealth Alliance, a group that seeks to protect humanity from viruses that might jump from other species. "Most emerging human viruses come from wildlife, and these represent a significant threat to public health and biosecurity in the US and globally, as was demonstrated by the SARS coronavirus pandemic of 2002-03," he wrote in the project's Public Health Relevance Statement. "This project seeks to understand what factors allow coronaviruses, including close relatives to SARS, to evolve and jump into the human population by studying viral diversity in their animal reservoirs (bats), surveying people that live in high-risk communities in China for evidence of bat-coronavirus infection, and conducting laboratory experiments to analyze and predict which newly-discovered viruses pose the greatest threat to human health." Since gain-of-function research was effectively banned in the United States, EcoHealth Alliance contracted with the Wuhan Institute of Virology in Wuhan to study coronaviruses found in bats in the Yunnan province…the very same bats that have the strain of coronavirus that is closest to SARS-CoV-2. The Wuhan Institute of Virology vehemently denies performing any gain-of-function experiments, but since Dr. Zhengli's files are sealed, it is impossible to know exactly how she was spending EcoHealth Alliance's grant money. Dr. Zhengli herself has come under fire for "unsafe laboratory practices" that may have allowed SARS-CoV-2 to escape. As far back as 2018, a cable from the U.S. Embassy in Beijing warned that "during interactions with scientists at the Wuhan Institute of Virology laboratory, they noted the new lab has a serious shortage of appropriately trained technicians and investigators needed to safely operate this high-containment laboratory." Dr. Zhengling has admitted that she did not perform coronavirus research in biosafety level-4 areas that require hazardous materials suits and extreme precautions. Instead, she said she worked in a biosafety level-2 lab, which requires only moderate precautions. On balance, which seems more likely: That a virus escaped from a lab that was performing experiments in known unsafe conditions or that a bat somehow traveled 1,000 miles from the caves of Yunnan to the Wuhan wet market and bit someone? All Gallagher wants is a further investigation of what is looking likelier and likelier by the day—that the virus escaped from the lab and the Chinese government is trying to cover up its embarrassing slip-up… just like it tries to cover up all of its embarrassing slip-ups. |
| You are subscribed to email updates from "sars transmission,sars treatment,sars virus origin" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |

Comments
Post a Comment