“Types and stages of COPD: Symptoms, causes, and more - Medical News Today” plus 1 more
“Types and stages of COPD: Symptoms, causes, and more - Medical News Today” plus 1 more |
| Types and stages of COPD: Symptoms, causes, and more - Medical News Today Posted: 20 Jan 2021 12:00 AM PST 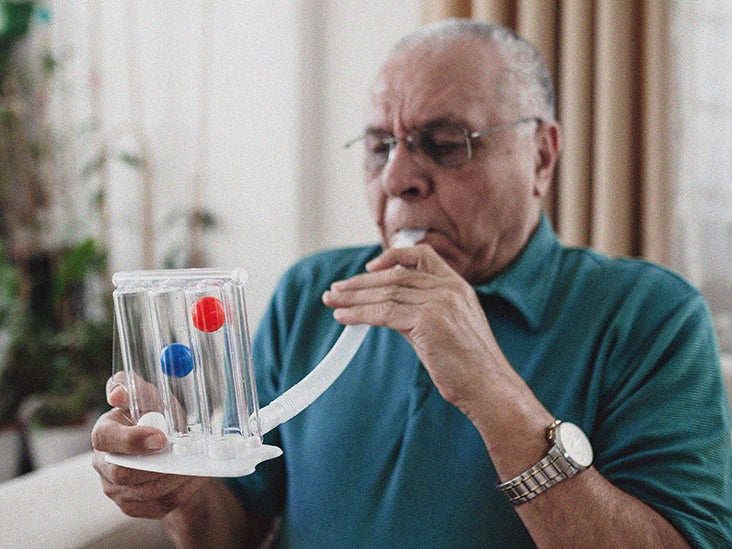 The main types of chronic obstructive pulmonary disease (COPD) are emphysema and chronic bronchitis. They differ in the kind of damage they do to the airways and lungs. However, the causes, symptoms, and treatment of the two conditions are almost completely identical. There are four stages of COPD that range from mild to very severe. A person with mild COPD may not know that they have the condition, while someone with very severe COPD will experience life threatening symptoms. Keep reading to learn about the types and stages of COPD, including causes, symptoms, and treatment options. COPD refers to a group of diseases that cause breathing problems and blockages in airflow. They gradually get worse over time. According to the Centers for Disease Control and Prevention (CDC), nearly 15.7 million people in the United States have a diagnosis of COPD. The CDC add that COPD is more common in:
A person's windpipe connects to the lungs, where it divides into many smaller branches. These branches end in small air sacs called alveoli, which have tiny blood vessels known as capillaries running along their walls. Here, oxygen passes from the sacs into the capillaries, and the waste product carbon dioxide passes from the capillaries into the sacs. Breathing involves this exchange of gases. In someone with healthy lungs, the airways and air sacs are stretchy. This elasticity permits the sacs to inflate when a person breathes in and deflate when they breathe out. People with COPD have less air going in and out of their airways because of one or more of the following:
The two main types of COPD are emphysema and chronic bronchitis, but many individuals with COPD can have both. EmphysemaIn emphysema, the alveoli, which are the walls of the air sacs, and the small airways suffer damage. As a result of this damage, the sacs lose their shape and ability to recoil during the expiratory phase of the breathing cycle, resulting in trapped air in the lung. This trapped air continues to distend the alveoli, causing a repeating cycle of airway obstruction. These changes eventually result in the lungs becoming hyperinflated, which reduces the exchange of gases. This makes it difficult for people to breathe and oxygenate their blood effectively while impairing the ability to breathe out carbon dioxide from the blood. Chronic bronchitisIn chronic bronchitis, the lining of the airways stays inflamed. This leads to swelling and the formation of large amounts of mucus. These effects make it hard to breathe. Learn more about the differences between emphysema and chronic bronchitis here. Below we describe the stages of COPD. There are multiple classification systems used in diagnosing COPD conditions. The following stages come from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, which derive from a specific breathing test called spirometry grading. However, this type of testing only captures one component of COPD severity. For example, two patients with the same result may have different tolerances to exercise, symptoms, and prognoses. Therefore, other COPD aspects, such as the severity of symptoms, risk of exacerbations, and presence of comorbidities, are important to the patient's experience of the disease and prognosis.
According to the National Heart, Lung, and Blood Institute (NHLBI), the leading cause of emphysema and chronic bronchitis involves long-term exposure to substances that irritate the airways and lungs. The NHLBI note that the primary sources of irritants include tobacco smoke from:
The following irritants can also play a role in the development of COPD:
In addition, a genetic condition called alpha-1 antitrypsin deficiency may play a role in developing emphysema. It involves reduced production of a protein that protects the lungs. Symptoms of emphysema or chronic bronchitis include:
Aside from the above, some people may have frequent colds and flu. If COPD is severe, symptoms may include:
While emphysema and chronic bronchitis have no cure, lifestyle changes and medical treatments can help a person feel better and delay the worsening of conditions. MedicationMedications can include bronchodilator inhalers, which relax the muscles surrounding the airways, making it easier to breathe. Below, the NHLBI note the type of inhalers appropriate for different stages:
VaccinesBecause respiratory infections can cause serious problems for individuals with COPD, doctors may recommend getting vaccines to reduce their risk. These include the flu and pneumonia vaccines. Oxygen therapyOxygen therapy can help people with severe COPD, accord to the NHLBI. A person on this treatment receives the oxygen through a mask or nasal prongs. The NHLBI list the following benefits from this treatment:
SurgeryA lung transplant is a last resort for people with one of the main types of COPD. If a person has emphysema, they have other surgical options, including:
Lifestyle changesQuitting smoking is the most important thing someone with COPD can do. If individuals find this challenging, they may wish to join a support group. They may also consider asking their family and friends for additional support. It is also helpful for them to avoid secondhand smoke and other irritants in their environment. People with COPD may have difficulties in eating enough because of their symptoms. If so, they can talk with their doctor about recommendations to help them get enough nutrition. For example, a healthcare professional may advise eating smaller, more frequent meals. Another lifestyle-related measure involves attending pulmonary rehabilitation, a personalized program that teaches management strategies. The plan may include instruction in breathing techniques and ways to conserve energy. The two primary types of COPD are emphysema and chronic bronchitis. The four stages of COPD range from mild to very severe. Some symptoms may include an ongoing cough, shortness of breath, and wheezing. A primary cause of both COPD types is long-term exposure to tobacco smoke, so doctors strongly urge people with the conditions to stop smoking. In addition to this, lifestyle changes, such as quitting smoking, or treatments, such as medications and oxygen therapy, can also help. |
| Posted: 02 Feb 2021 12:00 AM PST  Boston, Mass. - COVID-19 has caused more than 2 million deaths worldwide since the World Health Organization declared it a pandemic in March 2020. Patients with severe COVID-19 frequently experience respiratory distress and require assistance breathing. For patients whose lungs are so injured that even a ventilator is unable to deliver enough oxygen, extracorporeal membrane oxygenation (ECMO) -- which does the work of the lungs by removing carbon dioxide and adding oxygen to blood outside the body -- may improve the odds of survival for certain patients with severe COVID-19. A study by physician-researchers at Beth Israel Deaconess Medical Center (BIDMC) and Brigham and Women's Hospital (BWH) provides new evidence that critically ill patients with COVID-19 who were treated with ECMO had better odds of survival than those who were not treated with ECMO. The findings -- published in Intensive Care Medicine [LINK] -- represent the only published study to investigate ECMO's efficacy for treatment of critically ill patients with COVID-19. "ECMO gives patients' lungs time to heal when we've exhausted every other aspect of care for these patients -- it can be a bridge to recovery," said corresponding author Shahzad Shaefi, MD, Co-Director of the ECMO Program at BIDMC and in the Department of Anesthesia, Critical Care and Pain Medicine. "But ECMO's efficacy in the context of COVID-19 remains unclear. This work sheds new light on that question in the most robust way possible during the COVID-19 pandemic." The team analyzed observational data from Study of the Treatment and Outcomes in Critically Ill Patients with COVID-19 (STOP-COVID), a multicenter cohort study of patients with COVID-19 admitted to intensive care units at 68 hospitals across the United States. Spearheaded in March 2020 by senior author David E. Leaf, MD, Director of Clinical and Translational Research in Acute Kidney Injury in the Division of Renal Medicine at the Brigham, the STOP-COVID dataset includes more than 5,000 critically ill adult patients and depended on a dedicated volunteer workforce to collect more than 800 individual data elements per patient, all by manual chart review. "This was a remarkable grassroots effort involving more than 400 research assistants, medical students, residents, fellows, and attendings across the United States collecting this data manually during the height of the pandemic," said Leaf, who is also Assistant Professor of Medicine at Harvard Medical School. "People were highly motivated to get this database assembled, as it represents the best data we have about critically ill patients with COVID-19 in this country." Overall, the scientists found that 190 of the 5,122 critically ill adults (3 percent) admitted to the ICU with COVID-19 between March 1 and July 1, 2020, received treatment with ECMO. Among those 190 patients, nearly 70 percent survived to hospital discharge or at least 60 days following ICU admission. Next, Shaefi, Leaf and colleagues delved deeper into the data using an analytic technique called target trial emulation, which allows researchers to use observational data to infer causality when randomized controlled trials are unavailable. By this method, the researchers examined selected patients with severe respiratory failure, defined as those with a very low ratio of oxygen content in their blood divided by the amount of inspired oxygen delivered by the ventilator. They found that patient treated with ECMO in the first seven days of ICU admission had a considerable reduction in mortality compared to those who were similarly ill but who were not treated with ECMO. Specifically, among the 1,297 patients eligible for the target trial emulation, just over a third of the 130 who received ECMO died, compared to nearly half of those who did not receive ECMO. "These findings are not only statistically significant, but very clinically meaningful," said Leaf. "They show a considerable magnitude of benefit with ECMO - a 45 percent reduction in death - among the sickest patients. That's very compelling evidence that ECMO saves lives." "The real question with ECMO is, are we saving lives, or -- candidly -- are we prolonging poor outcomes and death," said Shaefi, who is also Assistant Professor in Anesthesia at Harvard Medical School. "The benefit of ECMO prevailed across all of our analyses. In the absence of a randomized controlled trial, which traditionally been very difficult to cleanly do in ECMO, this work represents perhaps the best current evidence we have of the role of ECMO in treating select critically ill COVID 19 patients." ### In addition to Shaefi and Leaf, co-authors included, Brian P. O'Gara and Megan L. Krajewski of BIDMC; Shruti Gupta, Tanveer Shaukat, Harkarandeep Singh, and Wei Wang of BWH. Please see the publication for a complete list of authors and affiliations. This study is unfunded work. DEL received research support from BioPorto outside the submitted work. SG is a scientific coordinator for the ASCEND trial (GlaskoSmithKline), outside the submitted work. BOG receives consulting fees from Sedana Medical outside the submitted work. Please see the paper for a complete list of author disclosures. The authors of the writing committee are supported by the following grants from the National Institute of Health (grants K08GM134220 and R03AG060179 (SS); R01HL144566 and R01DK125786 (DEL); K23HL130648 (KSM); R37 AI102634 (MAH); F32DC017342 (SG); K23DK120811(AS); K23HL143053 (MWS). Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system. |
| You are subscribed to email updates from "respiratory drugs,respiratory failure causes,respiratory failure treatment" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment