“Severe Acute Respiratory Distress Syndrome Secondary to Coronavirus 2 (SARS-CoV-2) - DocWire News” plus 3 more
“Severe Acute Respiratory Distress Syndrome Secondary to Coronavirus 2 (SARS-CoV-2) - DocWire News” plus 3 more |
- Severe Acute Respiratory Distress Syndrome Secondary to Coronavirus 2 (SARS-CoV-2) - DocWire News
- Virology, transmission, and pathogenesis of SARS-CoV-2 - The BMJ
- Convalescent plasma therapy in COVID-19: A double edged sword - The BMJ
- Tocilizumab fails to affect COVID-19 disease outcomes in Boston trial - News-Medical.Net
| Severe Acute Respiratory Distress Syndrome Secondary to Coronavirus 2 (SARS-CoV-2) - DocWire News Posted: 23 Oct 2020 11:00 PM PDT  Int J Occup Environ Med. 2020 Oct;11(4):157-178. doi: 10.15171/ijoem.2019.2202. ABSTRACT The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes coronavirus disease 2019 (COVID-19) and has created a worldwide pandemic. Many patients with this infection have an asymptomatic or mild illness, but a small percentage of patients require hospitalization and intensive care. Patients with respiratory tract involvement have a spectrum of presentations that range from scattered ground-glass infiltrates to diffuse infiltrates with consolidation. Patients with the latter radiographic presentation have severe hypoxemia and usually require mechanical ventilation. In addition, some patients develop multiorgan failure, deep venous thrombi with pulmonary emboli, and cytokine storm syndrome. The respiratory management of these patients should focus on using low tidal volume ventilation with low intrathoracic pressures. Some patients have significant recruitable lung and may benefit from higher positive end-expiratory pressure (PEEP) levels and/or prone positioning. There is no well-established anti-viral treatment for this infection; the United States Food and Drug Administration (FDA) has provided emergency use authorization for convalescent plasma and remdesivir for the treatment of patients with COVID-19. In addition, randomized trials have demonstrated that dexamethasone improves outcomes in patients on mechanical ventilators or on oxygen. There are ongoing trials of other drugs which have the potential to moderate the acute inflammatory state seen in some of these patients. These patients often need prolonged high-level intensive care. Hospitals are confronted with significant challenges in patient management, supply management, health care worker safety, and health care worker burnout. PMID:33098401 | DOI:10.15171/ijoem.2019.2202 |
| Virology, transmission, and pathogenesis of SARS-CoV-2 - The BMJ Posted: 23 Oct 2020 02:28 AM PDT
What you need to know
Since the emergence of SARS-CoV-2 in December 2019, there has been an unparalleled global effort to characterise the virus and the clinical course of disease. Coronavirus disease 2019 (covid-19), caused by SARS-CoV-2, follows a biphasic pattern of illness that likely results from the combination of an early viral response phase and an inflammatory second phase. Most clinical presentations are mild, and the typical pattern of covid-19 more resembles an influenza-like illness—which includes fever, cough, malaise, myalgia, headache, and taste and smell disturbance—rather than severe pneumonia (although emerging evidence about long term consequences is yet to be understood in detail).1 In this review, we provide a broad update on the emerging understanding of SARS-CoV-2 pathophysiology, including virology, transmission dynamics, and the immune response to the virus. Any of the mechanisms and assumptions discussed in the article and in our understanding of covid-19 may be revised as further evidence emerges. What we know about the virusSARS-CoV-2 is an enveloped β-coronavirus, with a genetic sequence very similar to SARS-CoV-1 (80%) and bat coronavirus RaTG13 (96.2%).2 The viral envelope is coated by spike (S) glycoprotein, envelope (E), and membrane (M) proteins (fig 1). Host cell binding and entry are mediated by the S protein. The first step in infection is virus binding to a host cell through its target receptor. The S1 sub-unit of the S protein contains the receptor binding domain that binds to the peptidase domain of angiotensin-converting enzyme 2 (ACE 2). In SARS-CoV-2 the S2 sub-unit is highly preserved and is considered a potential antiviral target. The virus structure and replication cycle are described in figure 1. Fig 1 (1) The virus binds to ACE 2 as the host target cell receptor in synergy with the host's transmembrane serine protease 2 (cell surface protein), which is principally expressed in the airway epithelial cells and vascular endothelial cells. This leads to membrane fusion and releases the viral genome into the host cytoplasm (2). Stages (3-7) show the remaining steps of viral replication, leading to viral assembly, maturation, and virus release Coronaviruses have the capacity for proofreading during replication, and therefore mutation rates are lower than in other RNA viruses. As SARS-CoV-2 has spread globally it has, like other viruses, accumulated some mutations in the viral genome, which contains geographic signatures. Researchers have examined these mutations to study virus characterisation and understand epidemiology and transmission patterns. In general, the mutations have not been attributed to phenotypic changes affecting viral transmissibility or pathogenicity. The G614 variant in the S protein has been postulated to increase infectivity and transmissibility of the virus.3 Higher viral loads were reported in clinical samples with virus containing G614 than previously circulating variant D614, although no association was made with severity of illness as measured by hospitalisation outcomes.3 These findings have yet to be confirmed with regards to natural infection. Why is SARS-CoV-2 more infectious than SARS-CoV-1?SARS-CoV-2 has a higher reproductive number (R0) than SARS-CoV-1, indicating much more efficient spread.1 Several characteristics of SARS-CoV-2 may help explain this enhanced transmission. While both SARS-CoV-1 and SARS-CoV-2 preferentially interact with the angiotensin-converting enzyme 2 (ACE 2) receptor, SARS-CoV-2 has structural differences in its surface proteins that enable stronger binding to the ACE 2 receptor4 and greater efficiency at invading host cells.1 SARS-CoV-2 also has greater affinity (or bonding) for the upper respiratory tract and conjunctiva,5 thus can infect the upper respiratory tract and conduct airways more easily.6 Viral load dynamics and duration of infectiousnessViral load kinetics could also explain some of the differences between SARS-CoV-2 and SARS-CoV-1. In the respiratory tract, peak SARS-CoV-2 load is observed at the time of symptom onset or in the first week of illness with subsequent decline thereafter, which indicates the highest infectiousness potential just before or within the first five days of symptom onset (fig 2).7 In contrast, in SARS-CoV-1 the highest viral loads were detected in the upper respiratory tract in the second week of illness, which explains its minimal contagiousness in the first week after symptom onset, enabling early case detection in the community.7 Fig 2 After the initial exposure, patients typically develop symptoms within 5-6 days (incubation period). SARS-CoV-2 generates a diverse range of clinical manifestations, ranging from mild infection to severe disease accompanied by high mortality. In patients with mild infection, initial host immune response is capable of controlling the infection. In severe disease, excessive immune response leads to organ damage, intensive care admission, or death. The viral load peaks in the first week of infection, declines thereafter gradually, while the antibody response gradually increases and is often detectable by day 14 (figure adapted with permission from doi:10.1016/j.cell.2020.04.013; doi:10.1016/S2213-2600(20)30230-7) Quantitative reverse transcription polymerase chain reaction (qRT-PCR) technology can detect viral SARS-CoV-2 RNA in the upper respiratory tract for a mean of 17 days (maximum 83 days) after symptom onset.7 However, detection of viral RNA by qRT-PCR does not necessarily equate to infectiousness, and viral culture from PCR positive upper respiratory tract samples has been rarely positive beyond nine days of illness.5 This corresponds to what is known about transmission based on contact tracing studies, which is that transmission capacity is maximal in the first week of illness, and that transmission after this period has not been documented.8 Severely ill or immune-compromised patients may have relatively prolonged virus shedding, and some patients may have intermittent RNA shedding; however, low level results close to the detection limit may not constitute infectious viral particles. While asymptomatic individuals (those with no symptoms throughout the infection) can transmit the infection, their relative degree of infectiousness seems to be limited.91011 People with mild symptoms (paucisymptomatic) and those whose symptom have not yet appeared still carry large amounts of virus in the upper respiratory tract, which might contribute to the easy and rapid spread of SARS-CoV-2.7 Symptomatic and pre-symptomatic transmission (one to two days before symptom onset) is likely to play a greater role in the spread of SARS-CoV-2.1012 A combination of preventive measures, such as physical distancing and testing, tracing, and self-isolation, continue to be needed. Route of transmission and transmission dynamicsLike other coronaviruses, the primary mechanism of transmission of SARS-CoV-2 is via infected respiratory droplets, with viral infection occurring by direct or indirect contact with nasal, conjunctival, or oral mucosa. Target host receptors are found mainly in the human respiratory tract epithelium, including the oropharynx and upper airway. The conjunctiva and gastrointestinal tracts are also susceptible to infection and may serve as transmission portals.6 Transmission risk depends on factors such as contact pattern, environment, infectiousness of the host, and socioeconomic factors, as described elsewhere.12 Most transmission occurs through close range contact (15 minutes face to face and within 2 m),13 and spread is especially efficient within households and through gatherings of family and friends.12 Household secondary attack rates (the proportion of susceptible individuals who become infected within a group of susceptible contacts with a primary case) ranges from 4% to 35%.12 Sleeping in the same room as, or being a spouse of an infected individual increases the risk of infection, but isolation of the infected person away from the family is related to lower risk of infection.12 Other activities identified as high risk include dining in close proximity with the infected person, sharing food, and taking part in group activities 12 The risk of infection substantially increases in enclosed environments compared with outdoor settings.12 Aerosol transmission can still factor during prolonged stay in crowded, poorly ventilated indoor settings (meaning transmission could occur at a distance >2 m).12141516 The role of faecal shedding in SARS-CoV-2 transmission and the extent of fomite (through inanimate surfaces) transmission also remain to be fully understood. Both SARS-CoV-2 and SARS-CoV-1 remain viable for many days on smooth surfaces (stainless steel, plastic, glass) and at lower temperature and humidity (eg, air conditioned environments).1718 Thus, transferring infection from contaminated surfaces to the mucosa of eyes, nose, and mouth via unwashed hands is a possible route of transmission. This route of transmission may contribute especially in facilities with communal areas, with increased likelihood of environmental contamination. However, both SARS-CoV-1 and SARS-CoV-2 are readily inactivated by commonly used disinfectants, emphasising the potential value of surface cleaning and handwashing. SARS-CoV-2 RNA has been found in stool samples and RNA shedding often persists for longer than in respiratory samples7; however, virus isolation has rarely been successful from the stool.57 No published reports describe faecal-oral transmission. In SARS-CoV-1, faecal-oral transmission was not considered to occur in most circumstances; but, one explosive outbreak was attributed to aerosolisation and spread of the virus across an apartment block via a faulty sewage system.19 It remains to be seen if similar transmission may occur with SARS-CoV-2. PathogenesisViral entry and interaction with target cellsSARS-CoV-2 binds to ACE 2, the host target cell receptor.1 Active replication and release of the virus in the lung cells lead to non-specific symptoms such as fever, myalgia, headache, and respiratory symptoms.1 In an experimental hamster model, the virus causes transient damage to the cells in the olfactory epithelium, leading to olfactory dysfunction, which may explain temporary loss of taste and smell commonly seen in covid-19.20 The distribution of ACE 2 receptors in different tissues may explain the sites of infection and patient symptoms. For example, the ACE 2 receptor is found on the epithelium of other organs such as the intestine and endothelial cells in the kidney and blood vessels, which may explain gastrointestinal symptoms and cardiovascular complications.21 Lymphocytic endotheliitis has been observed in postmortem pathology examination of the lung, heart, kidney, and liver as well as liver cell necrosis and myocardial infarction in patients who died of covid-19.122 These findings indicate that the virus directly affects many organs, as was seen in SARS-CoV-1 and influenzae. Much remains unknown. Are the pathological changes in the respiratory tract or endothelial dysfunction the result of direct viral infection, cytokine dysregulation, coagulopathy, or are they multifactorial? And does direct viral invasion or coagulopathy directly contribute to some of the ischaemic complications such as ischaemic infarcts? These and more, will require further work to elucidate. Immune response and disease spectrum (figure 2)After viral entry, the initial inflammatory response attracts virus-specific T cells to the site of infection, where the infected cells are eliminated before the virus spreads, leading to recovery in most people.23 In patients who develop severe disease, SARS-CoV-2 elicits an aberrant host immune response.2324 For example, postmortem histology of lung tissues of patients who died of covid-19 have confirmed the inflammatory nature of the injury, with features of bilateral diffuse alveolar damage, hyaline-membrane formation, interstitial mononuclear inflammatory infiltrates, and desquamation consistent with acute respiratory distress syndrome (ARDS), and is similar to the lung pathology seen in severe Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS).2526 A distinctive feature of covid-19 is the presence of mucus plugs with fibrinous exudate in the respiratory tract, which may explain the severity of covid-19 even in young adults.27 This is potentially caused by the overproduction of pro-inflammatory cytokines that accumulate in the lungs, eventually damaging the lung parenchyma.23 Some patients also experience septic shock and multi-organ dysfunction.23 For example, the cardiovascular system is often involved early in covid-19 disease and is reflected in the release of highly sensitive troponin and natriuretic peptides.28 Consistent with the clinical context of coagulopathy, focal intra-alveolar haemorrhage and presence of platelet-fibrin thrombi in small arterial vessels is also seen.26 Cytokines normally mediate and regulate immunity, inflammation, and haematopoiesis; however, further exacerbation of immune reaction and accumulation of cytokines in other organs in some patients may cause extensive tissue damage, or a cytokine release syndrome (cytokine storm), resulting in capillary leak, thrombus formation, and organ dysfunction.2329 Mechanisms underlying the diverse clinical outcomesClinical outcomes are influenced by host factors such as older age, male sex, and underlying medical conditions,1 as well as factors related to the virus (such as viral load kinetics), host-immune response, and potential cross-reactive immune memory from previous exposure to seasonal coronaviruses (box 1). Box 1 Risk factors associated with the development of severe disease, admission to intensive care unit, and mortalityUnderlying conditionPresentationLaboratory markersSex-related differences in immune response have been reported, revealing that men had higher plasma innate immune cytokines and chemokines at baseline than women.30 In contrast, women had notably more robust T cell activation than men, and among male participants T cell activation declined with age, which was sustained among female patients. These findings suggest that adaptive immune response may be important in defining the clinical outcome as older age and male sex is associated with increased risk of severe disease and mortality. Increased levels of pro-inflammatory cytokines correlate with severe pneumonia and increased ground glass opacities within the lungs.2931 In people with severe illness, increased plasma concentrations of inflammatory cytokines and biomarkers were observed compared with people with non-severe illness.293233 Emerging evidence suggests a correlation between viral dynamics, the severity of illness, and disease outcome.7 Longitudinal characteristics of immune response show a correlation between the severity of illness, viral load, and IFN- α, IFN-γ, and TNF-α response.33 In the same study many interferons, cytokines, and chemokines were elevated early in disease for patients who had severe disease and higher viral loads. This emphasises that viral load may drive these cytokines and the possible pathological roles associated with the host defence factors. This is in keeping with the pathogenesis of influenza, SARS, and MERS whereby prolonged viral shedding was also associated with severity of illness.734 Given the substantial role of the immune response in determining clinical outcomes, several immunosuppressive therapies aimed at limiting immune-mediated damage are currently in various phases of development (table 1). Table 1 Therapeutics currently under investigation View this table: Immune response to the virus and its role in protectionCovid-19 leads to an antibody response to a range of viral proteins, but the spike (S) protein and nucleocapsid are those most often used in serological diagnosis. Few antibodies are detectable in the first four days of illness, but patients progressively develop them, with most achieving a detectable response after four weeks.35 A wide range of virus-neutralising antibodies have been reported, and emerging evidence suggests that these may correlate with severity but wane over time.36 The duration and protectivity of antibody and T cell responses remain to be defined through studies with longer follow-up. CD-4 T cell responses to endemic human coronaviruses appear to manifest cross-reactivity with SARS-CoV-2, but their role in protection remains unclear.37 Unanswered questionsFurther understanding of the pathogenesis for SARS-CoV-2 will be vital in developing therapeutics, vaccines, and supportive care modalities in the treatment of covid-19. More data are needed to understand the determinants of healthy versus dysfunctional response and immune markers for protection and the severity of disease. Neutralising antibodies are potential correlates of protection, but other protective antibody mechanisms may exist. Similarly, the protective role of T cell immunity and duration of both antibody and T cell responses and the correlates of protection need to be defined. In addition, we need optimal testing systems and technologies to support and inform early detection and clinical management of infection. Greater understanding is needed regarding the long term consequences following acute illness and multisystem inflammatory disease, especially in children. Education into practiceHow would you describe SARS-CoV-2 transmission routes and ways to prevent infection? How would you describe to a patient why cough, anosmia, and fever occur in covid-19? Questions for future research
How patients were involved in the creation of this articleNo patients were directly involved in the creation of this article. How this article was createdWe searched PubMed from 2000 to 18 September 2020, limited to publications in English. Our search strategy used a combination of key words including "COVID-19," "SARS-CoV-2," "SARS", "MERS," "Coronavirus," "Novel Coronavirus," "Pathogenesis," "Transmission," "Cytokine Release," "immune response," "antibody response." These sources were supplemented with systematic reviews. We also reviewed technical documents produced by the Centers for Disease Control and Prevention and World Health Organization technical documents. Footnotes
This article is made freely available for use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained. https://bmj.com/coronavirus/usage |
| Convalescent plasma therapy in COVID-19: A double edged sword - The BMJ Posted: 22 Oct 2020 12:00 AM PDT Dear Editor The PLACID trial has provided the scientific community with important findings which will refine the management protocols for COVID-19 patients. It has now been established on the basis of various studies that the cause of mortality in COVID-19 patients is cytokine storm and the systemic inflammatory response syndrome and not directly due to the SARS-CoV-2 virus [1]. SARS-CoV-2 has been shown to trigger a specific immune response, which then results in production and release of various kinds of cytokines which in addition to killing the virus also damage the normal tissues and organs resulting in the cytokine storm [2]. There is a small window period before the primary immune response is produced against the virus [3]. It was hypothesized that convalescent plasma therapy, if given in the early phase of the disease, the passive IgG antibodies will be able to neutralize the virus and thus prevent the cytokine response in the patient and result in reduced mortality in the patients. This hypothesis was further supported by the fact that a better outcome was seen in SARS patients when they were treated with convalescent plasma during the early phase of the disease [4,5]. In another study there was 0% mortality in COVID-19 patients treated before day 7 of hospitalization as compared to 10% mortality in patients treated after that duration [6]. In the PLACID trial it was seen that there is a higher rate of conversion to a negative result for SARS-Cov-2 on day 7 of enrolment in the interventional arm as compared to the control arm. Therefore, the antibodies present in the convalescent plasma were able to neutralize the virus. However, convalescent plasma therapy did not result in decrease in patient mortality or affect the disease progression. Convalescent plasma therapy can be a double edged sword. The non-neutralizing antibodies in the convalescent plasma help in the entry of the virus into macrophages. The virus multiplies rapidly in the macrophages and can produce a pro-inflammatory condition, thereby aggravating the cytokine storm [7]. There are reports of convalescent plasma induced acute respiratory distress syndrome in patients of Ebola virus disease [8]. This is especially important in the case of elderly patients who already have an age related mild inflammatory condition called "inflamm-aging" and are more susceptible to developing a cytokine storm after COVID-19 infection [9]. The main goal of management during the COVID-19 pandemic is to reduce mortality and achieve the maximum recovery rate. Further research needs to be done to study the effect of the use of convalescent plasma therapy on patient mortality if used within the first 7 days of onset of symptoms. The use of convalescent plasma therapy in critical patients wit COVID-19 in whom a cytokine storm has already kicked in should be reconsidered. References |
| Tocilizumab fails to affect COVID-19 disease outcomes in Boston trial - News-Medical.Net Posted: 25 Oct 2020 07:08 PM PDT The United States continues to site at the top of the list of countries most affected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic with over 8.6 million severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cases to date and over 225,000 deaths from COVID-19 disease. At the peak of the pandemic to date, more than 1,000 Americans died from COVID-19 each day. Multiple studies have shown that SARS-CoV-2 infection can cause a wide range of symptoms starting from asymptomatic to mild or severe disease in humans that can even require mechanical ventilation in the worst cases. In some patients, SARS-CoV-2 infection leads to hypoxemic respiratory failure caused by a severe inflammatory response called a 'cytokine storm.' Patients in this phase are shown to have significantly abnormal inflammatory markers, including elevated levels of serum interleukin-6 (IL-6), ferritin, and C-reactive protein. Since high serum IL-6 levels are associated with high SARS-CoV-2 viral load and severe disease leading to death, it was hypothesized that this inflammatory cascade might be interrupted by IL-6 receptor blockade. However, the efficacy of (IL-6) receptor blockade in hospitalized COVID-19 patients not receiving mechanical ventilation is not clear. 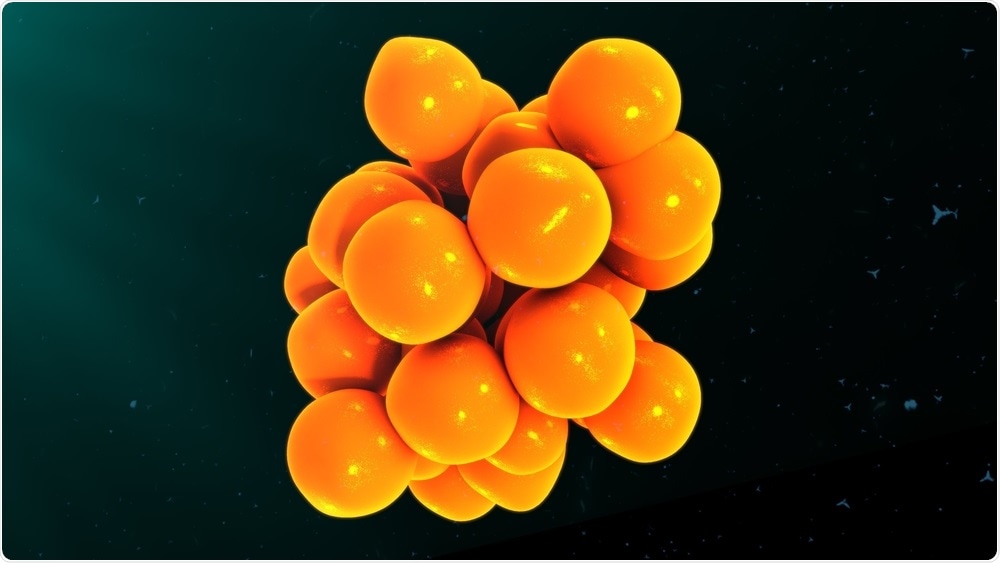 Cytokines 3d illustration. Image Credit: Sciencepics A randomized trial to determine the effects of IL-6 receptor blockade on COVID-19 progressionResearchers from the various Massachusetts hospitals performed the Boston Area COVID-19 Consortium (BACC) Bay Tocilizumab Trial using tocilizumab administered early in the disease course to determine if early IL-6 receptor blockade limits progression of COVID-19 to hypoxemic respiratory failure or death. Their work is published in the prestigious New England Journal of Medicine. The authors performed a randomized, double-blind, placebo-controlled trial in patients with SARS-CoV-2 infection, who showed hyperinflammatory signs and had at least 2 of the following symptoms: fever (>38°C), cannot maintain oxygen saturation >92% without supplemental oxygen, or pulmonary infiltrates. Patients received standard care and a single dose of either 8 mg / kg body weight of tocilizumab or placebo. The primary outcome was either intubation or death and was assessed in a time-to-event analysis. The secondary outcomes were clinical worsening and supplemental oxygen discontinuation, both determined by time-to-event analyses. Tocilizumab group had fewer serious infections compared to placebo groupThe study had 243 patients, out of which 102 (42%) were women, and 141 (58%) were men. The participants' median age was 59.8 years (range - 21.7 to 85.4), and 45% of the study cohort were Hispanic or Latino. The hazard ratio for intubation or death in patients who received tocilizumab compared with those who received a placebo was 0.83 (95% confidence interval [CI], 0.38 to 1.81; P = 0.64). The hazard ratio for the worsening of disease was 1.11 (95% CI, 0.59 to 2.10; P = 0.73). Eighteen percent of patients in the tocilizumab group and 14.9% of the participants in the placebo group experienced disease worsening at 14 days. The median time to supplemental oxygen discontinuation was 5 days (95% CI, 3.8 to 7.6) in patients who received tocilizumab and 4.9 days (95% CI, 3.8 to 7.8) in patients who received placebo (P=0.69). 24.6% of patients in the tocilizumab group and 21.2% in the placebo group were still receiving supplemental oxygen at 14 days. Patients on tocilizumab had fewer serious infections compared to patients who received a placebo. "Although tocilizumab did not show efficacy in this trial, the drug was not associated with excessive high-grade toxic effects in this population, which was characterized by multiple coexisting conditions." Tocilizumab not effective in affecting COVID-19 clinical outcomesThe study results proved that tocilizumab was not effective in preventing intubation or death in patients who were moderately ill and hospitalized with COVID-19. However, as the confidence intervals for efficacy comparisons were wide, the possibility of tocilizumab treatment causing some benefit or harm in some patients cannot be entirely ruled out. These results do not agree with the findings of multiple open-label trials, which suggested that IL-6 receptor blockade can play a significant role in preventing severe disease in COVID-19 patients. The authors say that although there is no clear explanation for the failure of tocilizumab to affect disease outcomes in their study, it is possible that patients with different demographic characteristics from the ones targeted by this trial may still benefit from IL-6 receptor blockade.
Journal reference: |
| You are subscribed to email updates from "what is respiratory distress,what is sars,what is sars virus" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |


Comments
Post a Comment