“Tracking an RSV Outbreak in the NICU Setting - Contagionlive.com” plus 2 more
“Tracking an RSV Outbreak in the NICU Setting - Contagionlive.com” plus 2 more |
- Tracking an RSV Outbreak in the NICU Setting - Contagionlive.com
- Covid 19 coronavirus: Flu vaccination strongly recommended during Covid-19 - New Zealand Herald
- Q & A on COVID-19 What is COVID-19? Why should the virus be closely - EU News
| Tracking an RSV Outbreak in the NICU Setting - Contagionlive.com Posted: 30 Apr 2020 07:21 AM PDT 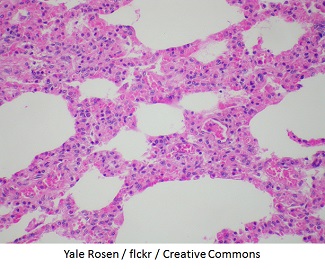 There were 2 distinct introductions of respiratory syncytial virus (RSV) in a neonatal intensive care unit (NICU) in an 11-day span, according to a paper published in the Journal of the Pediatric Infectious Disease Society. There were 2 distinct introductions of respiratory syncytial virus (RSV) in a neonatal intensive care unit (NICU) in an 11-day span, according to a paper published in the Journal of the Pediatric Infectious Disease Society.The Louisiana Department of Health was alerted to 7 RSV infections within a single NICU at a large, level III NICU with 5 wards in December 2017. Investigators, from the US Centers for Disease Control and Prevention (CDC), wrote the NICU is of particular concern for RSV outbreaks, due to the risk for severe disease in young infants, especially those born prematurely or with congenital abnormalities or other comorbidities, who encompass most of the NICU population. Investigators tracked the outbreak using whole genome sequencing to better understand the relatedness of viruses among the patients. The facility's visitation policy stipulated that parents are invited to stay overnight with their infant, the study authors wrote, and siblings over the age of 2 are allowed to visit during daytime hours; however, all guests must wash their hands prior to visitation. Additional guidelines are in place during flu season, which allow for guests' temperature checks upon entrance to the unit and barring any febrile visitors or those reporting respiratory symptoms from entering. Once the first patient was identified with RSV, the facility initiated enhanced surveillance for RSV, including nasopharyngeal specimen collection from NICU patients with respiratory or other RSV-related symptoms. Swabs were collected from all 7 patients within 2 days of symptom onset and initially tested at the hospital lab. They were sent to the CDC lab for further analysis, investigators wrote. Patient 1 was born at the facility and discharged 30 days prior to readmission. That infant was admitted to the NICU at age 34 days for acute respiratory distress. RSV infection was confirmed via PCR testing, and was considered day 0. Between days 1 8, the facility observed 6 additional patients with respiratory symptoms. They were diagnosed with RSV. Investigators wrote that RSV likely spread to new patients through shared staff and/or equipment. The rest of the patients were also born at the facility (preterm, ranging from 25 to 36 weeks) and none were on respiratory support prior to symptom onset. Investigators described the NICU patients: 6 were preterm and 1 had chronic lung disease. Additionally, 3 patients required respiratory support after symptom onset. None of the infants died, they said. The subsequent CDC lab tests showed that 6 of 7 infected patients were part of the same cluster. The seventh patient was admitted from the community presenting respiratory symptoms. That patient had a genetically distinct virus unrelated to the rest of the patients, the investigators determined. Aside from the 7 NICU patients who developed RSV, no other RSV infections were reported. All NICU health care workers were asked to report any respiratory symptoms at the start of their shift. No NICU health care workers reported any symptoms and none were tested for RSV, investigators wrote. Parents of NICU patients were informed of guidelines in place in the NICU through a letter. Additional precautions were initiated after discussion with the Louisiana Health Department and the CDC, including restricting visitation from children under 12 years, use of facemasks during visitation from nonstaff, increased hand hygiene, enhanced environmental cleaning, and cohorting of staff. "Policies that ban visitation by persons with respiratory symptoms and all young children when RSV is circulating may help prevent introduction of RSV into healthcare settings," investigators wrote. "This cluster also highlights the importance of early recognition of RSV, which should be considered when evaluating NICU patients for respiratory symptoms or sepsis, particularly during RSV season." To stay informed on the latest in infectious disease news and developments, please sign up for our weekly newsletter. |
| Covid 19 coronavirus: Flu vaccination strongly recommended during Covid-19 - New Zealand Herald Posted: 30 Apr 2020 05:25 PM PDT /arc-anglerfish-syd-prod-nzme.s3.amazonaws.com/public/HIQXC6K5SRCCNDFSE5OLQT6FGY.jpg) As New Zealanders unite to stop the spread of Covid-19, the Taranaki District Health Board (TDHB) is appealing to all residents to also unite against the influenza virus. As flu season approaches, Taranaki DHB's medical officer of health, Dr Jonathan Jarman, says although the influenza vaccine won't prevent Covid-19, it will help stop the spread of influenza. "One in four New Zealanders are infected with influenza every year. Many won't feel sick at all, but can still pass the virus onto family and co-workers." Both Covid-19 and influenza viruses cause illness of the nose, throat and airways, and are spread person to person through direct contact, cough and sneeze droplets and contaminated surfaces. Advertisement • Covid19.govt.nz: The Government's official Covid-19 advisory website Dr Jarman says getting an influenza vaccination will greatly lower a person's chances of catching the flu, reduce the chances of passing it on to others, and also help to reduce the load on the health system. "We don't want to have the hospital full of people with a preventable illness like influenza while we have the threat of Covid-19 hanging over us. "Each year we may encounter new types of influenza virus, so it's important to ensure we're vaccinated on an annual basis." Dr Jarman says influenza can be more than just a bad cold. "The flu is an infectious disease caused by an influenza virus and can affect anyone no matter how fit, active and healthy they may be. "Pregnant women, newborn babies, the elderly, people with lowered immunity and those with long term medical conditions such as asthma or heart problems are at higher risk of complications and hospitalisation from influenza." Symptoms can come on suddenly and include fever, chills, sore throat, muscle aches, headache, runny nose, cough, stomach upsets and severe fatigue. Advertisement "Influenza vaccination is safe, effective and can be lifesaving for those who are the most vulnerable. "I don't think anyone wants to catch a cough or cold this year because you won't know what it is." Anyone with symptoms should isolate and get tested for Covid-19, he says. "It is really important that anyone with a sniffle or a slight sore throat should go into isolation and get immediately tested for Covid-19." TDHB's general manager for Māori Health, Ngawai Henare, says Māori have the highest susceptibility to flu-related illness that ultimately places disproportionate demands on the health system. Vaccinating reduces the burden on whānau and on health services, she says. "While we've been working to vaccinate our vulnerable population early, we're encouraging everyone to get their flu shot in these weeks leading into winter." GPs and some pharmacies are currently offering vaccinations. Influenza vaccinations are free for eligible people including pregnant women, people aged 65 years or older, people aged under 65 years with diabetes, most heart or lung conditions and some other long-term illnesses. Children aged 4 years or under who have had a stay in hospital for asthma or other breathing problems are also eligible. |
| Q & A on COVID-19 What is COVID-19? Why should the virus be closely - EU News Posted: 24 Apr 2020 12:00 AM PDT  Medical information1. What are the symptoms of COVID-19 infectionSymptoms of COVID-19 vary in severity from having no symptoms at all (being asymptomatic) to having fever, cough, sore throat, general weakness and fatigue and muscular pain and in the most severe cases, severe pneumonia, acute respiratory distress syndrome, sepsis and septic shock, all potentially leading to death. Reports show that clinical deterioration can occur rapidly, often during the second week of disease. Recently, anosmia – loss of the sense of smell – (and in some cases the loss of the sense of taste) have been reported as a symptom of a COVID-19 infection. There is already evidence from South Korea, China and Italy that patients with confirmed SARS-CoV-2 infection have developed anosmia/hyposmia, in some cases in the absence of any other symptoms. 2. Are some people more at risk than others?Elderly people above 70 years of age and those with underlying health conditions (e.g. hypertension, diabetes, cardiovascular disease, chronic respiratory disease and cancer) are considered to be more at risk of developing severe symptoms. Men in these groups also appear to be at a slightly higher risk than females. See links to national guidelines on the treatment of patients with serious and life threatening conditions during COVID-19 under external resources 3. Are children also at risk of infection and what is their potential role in transmission?Children make up a very small proportion of reported COVID-19 cases, with about 1% of all cases reported being under 10 years, and 4% aged 10-19 years. Children appear as likely to be infected as adults, but they have a much lower risk than adults of developing symptoms or severe disease. There is still some uncertainty about the extent to which asymptomatic or mildly symptomatic children transmit disease. 4. What is the risk of infection in pregnant women and neonates?There is limited scientific evidence on the severity of illness in pregnant women after COVID-19 infection. It seems that pregnant women appear to experience similar clinical manifestations as non-pregnant women who have progressed to COVID-19 pneumonia and to date (as of 25 March), there have been no maternal deaths, no pregnancy losses and only one stillbirth reported. No current evidence suggests that infection with COVID-19 during pregnancy has a negative effect on the foetus. At present, there is no evidence of transmission of COVID-19 from mother to baby during pregnancy and only one confirmed COVID-19 neonatal case has been reported to date. ECDC will continue to monitor the emerging scientific literature on this question, and suggests that all pregnant women follow the same general precautions for the prevention of COVID-19, including regular handwashing, avoiding individuals who are sick, and self-isolating in case of any symptoms, while consulting a healthcare provider by telephone for advice. 5. Is there a treatment for the COVID-19 disease?There is no specific treatment or vaccine for this disease. Healthcare providers are mostly using a symptomatic approach, meaning they treat the symptoms rather than target the virus, and provide supportive care (e.g. oxygen therapy, fluid management) for infected persons, which can be highly effective. In severe and critically ill patients, a number of drugs are being tried to target the virus, but the use of these need to be more carefully assessed in randomised controlled trials. Several clinical trials are ongoing to assess their effectiveness but results are not yet available. As this is a new virus, no vaccine is currently available. Although work on a vaccine has already started by several research groups and pharmaceutical companies worldwide, it may be many months or even more than a year before a vaccine has been tested and is ready for use in humans. 6. When should I be tested for COVID-19?Current advice for testing depends on the stage of the outbreak in the country or area where you live. Testing approaches will be adapted to the situation at national and local level. National authorities may decide to test only subgroups of suspected cases based on the national capacity to test, the availability of necessary equipment for testing, the level of community transmission of COVID-19, or other criteria. As a resource conscious approach, ECDC has suggested that national authorities may consider prioritising testing in the following groups:
|
| You are subscribed to email updates from "infant respiratory distress syndrome symptoms,influenza,information about respiratory system" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment