“Vaccines Need Not Completely Stop COVID Transmission to Curb the Pandemic - Scientific American” plus 2 more
“Vaccines Need Not Completely Stop COVID Transmission to Curb the Pandemic - Scientific American” plus 2 more |
- Vaccines Need Not Completely Stop COVID Transmission to Curb the Pandemic - Scientific American
- What Happens When You Breathe - The New Yorker
- Mind-Blowing Facts About the Human Body You Never Knew - Integris
| Vaccines Need Not Completely Stop COVID Transmission to Curb the Pandemic - Scientific American Posted: 18 Jan 2021 03:47 AM PST 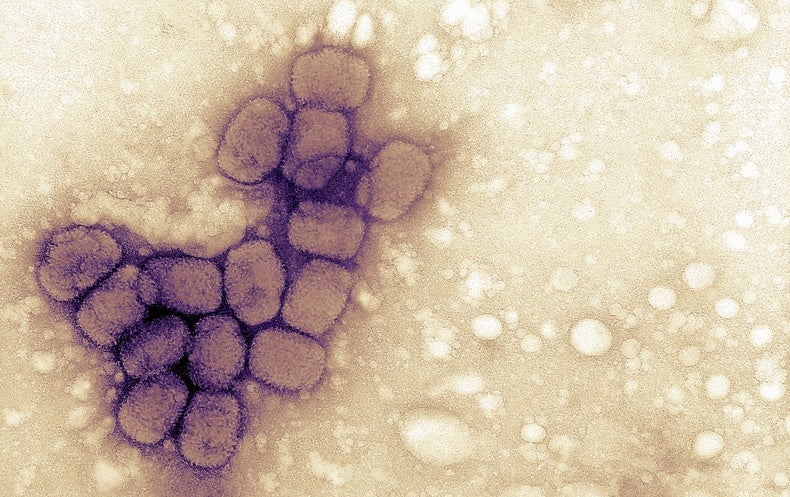 COVID-19 vaccine rollouts are finally upon us. They hope that herd immunity—protection from an infectious disease that occurs once a sufficient proportion of the population has been vaccinated or infected—is on the horizon. But even though the first vaccines to receive emergency use authorization from the U.S. Food and Drug Administration are exceptionally effective at preventing COVID-19, data cannot yet tell us if they hinder transmission of SARS-CoV-2, the virus that causes the disease. The question of whether immunization prevents recipients from becoming ill and from infecting others is not unique to the current pandemic. According to Dawn Bowdish, a professor of pathology and molecular medicine at McMaster University, this so-called sterilizing immunity was a key factor in eliminating smallpox. The smallpox, or variola, virus ravaged human populations for thousands of years, evidenced by traces of pustules found on the 3,000-year-old mummy of Egyptian pharaoh Ramses V. Reports indicate the virus was spreading globally by the first century C.E., and it eventually became a centuries-long pandemic. Historians think the disease killed more than 300 million people between 1900 and its official eradication in 1980. "Smallpox changed the history of the world—changing royal successions and the outcomes of wars that affected the destinies of whole countries," says Natasha Crowcroft, senior technical adviser for measles and rubella at the World Health Organization. The fight against smallpox inspired early inoculation efforts and led to English physician Edward Jenner's cowpox vaccine against smallpox in 1796. "The [smallpox] vaccination caused sterilizing immunity, meaning that you don't carry any of the virus. The antibodies that you generate, the responses you generate, clear the virus from your system entirely," Bowdish says. Although many vaccines widely used today (against measles, for example) produce very effective sterilizing immunity, others, such as the hepatitis B vaccine, do not. With these vaccines, an individual's immune system is trained to prevent illness, yet the pathogen can persist in that person's body, potentially allowing them to infect others. A lack of sterilizing immunity means that the pathogen can continue to circulate in a population, where it may cause illness in unvaccinated and vulnerable people or evolve to evade our immune responses, Bowdish explains. Sterilizing immunity may have been a lofty goal for COVID-19 vaccine manufacturers, though not necessary to curb disease. According to Crowcroft, the very concept of such immunity is nuanced. "In reality, the spectrum of protection might best be framed as the extent to which vaccination prevents transmission of the wild-type virus or bacteria," she says. The case of rotavirus—which causes severe vomiting and watery diarrhea and is especially dangerous to infants and young children—is fairly straightforward. Vaccination limits, but does not stop, the pathogen from replicating. As such, it does not protect against mild disease. By reducing an infected person's viral load, however, it decreases transmission, providing substantial indirect protection. According to the Centers for Disease Control, four to 10 years after the 2006 introduction of a rotavirus vaccine in the U.S., the number of positive tests for the disease fell by as much as 74 to 90 percent . The pathway to vaccine-mediated control of an infectious disease is not always so direct. Ultimately, whether, and to what degree, inoculation prevents transmission depends on the pathogen itself, the host or hosts it infects and the interaction between the two, Bowdish says. For example, vaccines against Bordetella pertussis, the primary bacterium that causes whooping cough, or pertussis, do a great job of preventing illness but do not entirely clear the pathogen. Rather, as B. pertussis replicates in the upper respiratory tract, vaccine-induced antibodies apply pressure via natural selection to weed out bacteria whose disease-causing genes are turned on. Because these same genes are responsible for the parts of the microorganisms that are targeted by antibodies, bacteria that keep them turned off evade the immune response and hang out undetected in the upper respiratory tract, Bowdish explains. This becomes a problem when someone with a naive immune system, such as an infant, contracts the pathogen. In the absence of antibodies, B. pertussis's disease-causing genes become activated again, causing illness. Nevertheless, the introduction of pertussis vaccines in the 1940s cut annual U.S. cases from more than 100,000 to fewer than 10,000 by 1965. In the 1980s cases began slowly climbing again as parents increasingly refused to vaccinate their children. Today there is renewed focus on reducing the chance of exposure and getting antibodies to infants by immunizing pregnant women and new mothers. Efforts to arrest the spread of polio provide additional insight into the complexity of stopping an epidemic. The two main categories of inoculations against polioviruses confer different types of immunity. The inactivated polio vaccine (IPV) protects against systemic infection and consequent paralysis but does not stop viral replication in the gut, so it offers no indirect protection to unvaccinated individuals. The oral polio vaccine (OPV) generates localized intestinal immunity, preventing infection and protecting against disease and transmission. Because the OPV uses a weakened live poliovirus, however, in rare cases among underimmunized populations, the attenuated virus mutates, circulates and once again causes illness. The Global Polio Eradication Initiative and the World Health Organization recommend distinct vaccination strategies depending on the local context. In places where wild polio still exists, OPV is key to slowing transmission. In areas where the wild virus has been eradicated, IPV keeps populations protected. Thanks to widespread immunization programs, the U.S. has been polio-free since 1979, and the disease is on the verge of global eradication. In a paper in the October 2020 issue of the American Journal of Preventive Medicine, researchers modeled what a COVID-19 vaccine with varying types of protection could mean. They found that if a vaccine protects 80 percent of those immunized and 75 percent of the population is vaccinated, it could largely end an epidemic without other measures such as social distancing. "Otherwise, you won't be able to rely on the vaccine to return us to 'normal,'" says Bruce Y. Lee, a co-author of the paper and a professor at the CUNY Graduate School of Public Health and Health Policy. That is, if the vaccine only prevents disease or reduces viral shedding rather than eliminating it, additional public health measures may still be necessary. Even so, Lee stressed that a widespread nonsterilizing vaccine could still reduce burden on the health care system and save lives. Influenza may provide the best blueprint of what to expect going forward. The most common flu vaccine—the inactivated virus—is not "truly sterilizing because it doesn't generate local immune response in the respiratory tract," Crowcroft says. This fact, coupled with low immunization rates (often shy of 50 percent among adults) and the influenza virus's ability to infect and move between multiple species, enables it to constantly change in ways that make it hard for our immune system to recognize. Still, depending on the year, flu vaccines have been shown to reduce hospitalizations among older adults by an estimated 40 percent and intensive care admissions of all adults by as much as 82 percent. Research on seasonal coronaviruses suggests that SARS-CoV-2 could similarly evolve to evade our immune systems and vaccination efforts, though probably at a slower pace. And data remain mixed on the relationship between symptoms, viral load and infectiousness. But ample precedent points to vaccines driving successful containment of infectious diseases even when they do not provide perfectly sterilizing immunity. "Measles, diphtheria, pertussis, polio, hepatitis B—these are all epidemic-prone diseases," Crowcroft says. "They show that we don't need 100 percent effectiveness at reducing transmission, or 100 percent coverage or 100 percent effectiveness against disease to triumph over infectious diseases." Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here. |
| What Happens When You Breathe - The New Yorker Posted: 18 Jan 2021 03:02 AM PST  For a man who died ninety-seven years ago, Carl Flügge had a very big 2020. We paid homage to him every time we waited in a socially distanced grocery line, used a homemade chute to deliver Halloween candy, or yelled "Six feet!" to a child wandering too close to a stranger. In an age of CRISPR and face transplants, one of the heroes of the coronavirus pandemic was a German doctor who, in 1897, measured how far bacteria-laden spittle could travel from the mouths of volunteers. Six feet, he determined, and so, last year, that became the recommendation offered by caution signs around the world. (In Sweden: "Please keep a distance about the size of a small moose between yourself and others.") We've learned that our breath can sometimes carry the coronavirus much farther than six feet, but the number is still useful and seems permanently etched into our brains. We are all Flüggeites now. Flügge was obsessed with hygiene, and for good reason. In his day, there was little to offer the sick in the way of effective medicines—beyond, say, opiates or quinine—and few vaccines were available. The best way to be of help, some physicians decided, was to try to find out how to keep patients from getting sick in the first place. At the time that Flügge was measuring droplet travel, New York City was overcome by a terrible respiratory disease. Tuberculosis, the city's leading killer, was claiming ten thousand lives a year. A local doctor, Hermann Biggs, proposed actions that he believed could save lives: reporting all TB patients to the health department, and tracking everyone with whom those patients had been in close contact. (Other physicians protested, calling the moves "aggressive tyrannies" and "offensively dictatorial," so Biggs wasn't able to implement them fully.) He also pushed for people to cover their mouths while coughing, and for patients infected with TB to be isolated from healthy people. Twenty years later, even with no advances in medication, Biggs's careful attention to the sharing of air had helped cut the number of TB cases in the city in half. Eventually, effective antibiotics were introduced, and by the nineteen-fifties TB was considered, in the United States, anyway, to have been more or less conquered by modern medicine. But, in the decades that followed, with the old precautions abandoned, the disease began to spread anew in New York, and there was an additional problem: incomplete treatment could lead to strains that resisted the drugs. The number of cases per capita doubled between 1980 and 1990. The pulmonologist Michael J. Stephen writes about the debacle in his wide-ranging new book, "Breath Taking: The Power, Fragility, and Future of Our Extraordinary Lungs" (Atlantic Monthly Press): "In a time when we had our most powerful antibiotics, New York was doing worse than Dr. Biggs had done ninety years before, with education and no antibiotics at all." The story is a reflection of the remarkable fact that, in the twentieth century, an era of astounding medical breakthroughs, simple—and relatively inexpensive—public-health interventions saved more lives than clinical medicine did. As a doctor of the lungs, Stephen is plenty interested in cutting-edge cancer therapies and treatments for such harrowing illnesses as cystic fibrosis, but he clearly sees his philosophical forebears in the likes of Biggs and Flügge—and even their successor William Wells, who, in the nineteen-thirties, introduced sneezing powder and Balantidium coli into the lecture halls and air-conditioners of the Harvard School of Public Health, just to find out how far the bacteria could travel and still reach human lungs. All of them understood a basic truth, which, Stephen maintains, becomes more profound the more you think about it: "The atmosphere is a communal space, and lungs are an extension of it." Our very breath ties us to one another and to the world around us. It's a lesson that we seem to struggle to remember. In countless languages and religions, breath is a synonym for life, as well as for the spirit or soul. And for good reason. The Earth spent some two billion years without oxygen in its atmosphere, bereft of life beyond a few anaerobic microorganisms. Slowly, blue-green algae generated a buildup of oxygen, and so created the conditions that allowed for the grand explosion of biology on which nearly everything and everyone we know depends. "Life and respiration are complementary," the English physician William Harvey wrote in the seventeenth century. "There is nothing living which does not breathe, nor anything breathing which does not live." He was overlooking anaerobes, of course, but the gist was right. Even plants respire, in a process separate from photosynthesis; animals such as jellyfish or earthworms, which lack respiratory systems, breathe through their skin. (A dried-up worm on the sidewalk is dead because it has suffocated.) Our very distant ancestors, having started with something more or less like a fish's swim bladder, developed lungs—a highly efficient mechanism for exchanging internal gases for atmospheric ones—and took to the land. It's a beginning we each reënact on the day we are born. Though other organs function in utero, independent life starts the moment that our fluid-filled lungs inflate, for the first time, with our own breath. And yet, Stephen argues, we have consistently overlooked the importance of our lungs (and not just by giving hearts all the glory in love songs). The details of our ordinary breathing—pacing, depth, and so on—get little attention in modern medicine, but Stephen tells us that breathing exercises, of the sort long promoted in Buddhism and Hinduism, may improve not just respiratory conditions but also depression and chronic pain. Some studies suggest that they can combat the damaging effects of stress; Stephen says that "mobilizing the power of the breath has also been shown to turn on anti-inflammatory genes and turn off pro-inflammatory ones, including genes that regulate energy metabolism, insulin secretion, and even the part of our DNA that controls longevity." The breath of life, indeed. Meanwhile, diseases of the lungs, which have often been stigmatized as "dirty," have trouble attracting research money and attention. ("Ignored, underfunded, and forgotten: this is the medical history of lung diseases," Stephen writes.) You've likely never heard of idiopathic pulmonary fibrosis, though it affects more Americans than cervical cancer and has a much lower survival rate. Lung cancer is by far the deadliest cancer in America, but other cancers receive significantly more funding. Even as deaths from traditional killers such as heart disease and cancer are largely in decline in the United States, mortality from respiratory diseases is rising. (And this was true before we lost hundreds of thousands of Americans to COVID-19, which kills most of its victims through acute respiratory failure.) Cases of asthma increase every year, and, globally, so do cases of chronic obstructive pulmonary disease, which is associated with smoking but also afflicts people who have never smoked. Lung cancer, too, is becoming more common among nonsmokers; in the United States, someone is diagnosed roughly every two and a half minutes. Worldwide, respiratory problems are the second most common cause of death, and the No. 1 killer of children under five. We tend to think of a lung as a simple pump: one gas is pulled in, another is pushed out. In fact, Stephen writes, "it is an organ alive with immunology and chemistry, one that does an extraordinary amount of work under extreme stress from the moment we enter this world." With each of the roughly twenty thousand breaths we take in a day, air travels through convoluted passages that can stretch for fifteen hundred miles, to one of the approximately five hundred million alveoli—tiny, clustered air sacs—that each of our lungs holds. Oxygen moves from the lungs to the bloodstream, as carbon dioxide flows back to the lungs. The brain stem controls the balance, which must be just right. Gas exchange has a remarkably immediate and intense effect on the body; one reason cigarettes are so addictive is the speed with which inhalation delivers drugs to the brain. When you hold your breath, what feels like hunger for oxygen is really your body's reaction to too much carbon dioxide, which turns blood acidic. When you breathe into a paper bag to quell a panic attack, it works because hyperventilating has tipped the balance in the other direction, leaving you without enough CO2. Lungs are a paradox. They are so fragile that an accumulation of the tiniest scars can rob them of their elasticity and function, so delicate that one of the pioneers of pulmonology solved a long-standing mystery about a deadly neonatal lung disease in part by reading a book about the physics of soap bubbles. Yet, unlike our other internal organs, nestled away inside us, they are open, like a wound, to the outside world. The respiratory system is regularly attacked by pathogens, to say nothing of allergens and pollutants. As a result, our lungs are home to vast numbers of protective cells that patrol them like sentries, and a lining of tiny hairs that constantly move a layer of cleansing mucus upward, ejecting all the invaders they can. Our lungs are both protection and portal, the nexus of our relationship with an environment that can heal us as well as harm us. In their deepest recesses, a wall as thin as a single cell is all that separates us from the world. In December of 1952, a temperature inversion, a relatively common wintertime meteorological event, developed in the skies above London, trapping cold air under a layer of warmer air. Because the air could not escape, the already terrible pollution of the city grew so concentrated that, in some areas, people could no longer see their feet. Buses and cabs stopped running because of the poor visibility, and some people blindly wandered into the Thames and drowned. The air quality was such that even indoor events had to be cancelled, and the press reported cows dying of asphyxiation. For five days, amid what became known as the Great Smog, Londoners got to know, too intimately, everything that the city emitted into the communal atmosphere—including coal smoke, from factories and homes, which mixed with fog and generated sulfuric acid. Enormous numbers of people were hospitalized, and, in the weeks and months that followed, an estimated twelve thousand died. Undertakers ran out of caskets. For centuries, there had been failed attempts to reduce coal burning in England—among them a ban in 1306 by Edward I, who turned to fines, torture, and death threats; and, in the sixteen-sixties, a report written for Charles II that warned about the effects of "filthy vapour" on "this frail Vessell of ours which contains it." But the region's famous air pollution was dismissed as simply the cost of modern life. Four years after the Great Smog, though, Britain finally passed a Clean Air Act and began its long, slow transition away from coal. (In 2020, Britain set a national record by going sixty-seven days, twenty-two hours, and fifty-five minutes without burning any coal for power—a first since the Industrial Revolution.) In the U.S., several years before the Great Smog, a winter inversion trapped the residents of Donora, Pennsylvania, in a cloud of emissions from local zinc and steel factories, sickening nearly half the town. The resulting outcry led to the first federal efforts to address air pollution, although America's Clean Air Act wasn't passed until 1963. People learned the hard way about the lack of separation between themselves and what they breathed. Or not. In today's world, episodes like the Great Smog are less famous but more common. In recent years, residents of cities from São Paulo to Sydney have watched as smoke from record fires, fuelled by climate change and deforestation, has blotted the sun from the sky. In November, 2017, air quality in New Delhi—a city that, like Seattle and Salt Lake City, is prone to winter inversions—was so bad that sensors tracking air pollution, including the level of particulates under 2.5 micrometres, which are small enough to travel deep into the lungs and even into the bloodstream, couldn't keep up. (Levels above 200 are considered "very unhealthy"; most sensors maxed out at 999.) Poor visibility caused a huge pileup of cars on a highway, and Delhi's chief minister tweeted that the region had become a gas chamber. But it wasn't an isolated event. Last winter, government officials in Delhi cancelled flights, shut down schools, and declared a health emergency because of air pollution. Millions of children are now believed to have irreversible lung damage, and a local surgeon told the Times that he no longer sees pink lungs, even among young nonsmokers. We're still learning all that air pollution can do to our bodies. It can cause not just lung diseases and impaired lung development (in Los Angeles, researchers found that they could track the progress of anti-pollution measures by the increasing size of children's lungs) but also, indirectly, heart attacks and osteoporosis. For first responders who breathed in clouds of dusty air following the 9/11 attacks on the World Trade Center, many of them without wearing protective masks, health problems often came in three waves. First, there were persistent coughs, and then, a few years later, asthma, sinus inflammation, acid-reflux disease, C.O.P.D., and pneumonia. Finally came cancer, heart disease, and stroke. In the U.S. today, our bad air comes not just from industry but from industrial agriculture (with its emissions of ammonia, hydrogen sulfide, methane, and the like); according to some research, the two cause about the same number of air-pollution-related deaths each year. Forty-six per cent of Americans live in counties where the air is considered unhealthy, raising the risk of disease and early death, with the brunt borne by poor people and people of color, who are likeliest to live in the most polluted areas. |
| Mind-Blowing Facts About the Human Body You Never Knew - Integris Posted: 18 Jan 2021 06:51 AM PST 01/18/2021  Your body is amazing. No, really! The human body is a complex structure of interconnected systems and vital organs that work day in and day out to fulfill the functions necessary for everyday living. For example, in order to eat, your mouth, esophagus, stomach, liver, pancreas, and intestines must work together in sync to break down and digest what you eat while extracting the nutrients necessary to keep you healthy. While most of us understand the basic bodily functions that keep us going, you might not be aware of some of the more incredible functions your body carries out. We've gathered up seven facts about the human body and some of its crazier processes that might blow your mind. Fact No. 1: Your gut is the only organ with its own independent nervous system.Your gastrointestinal system (commonly called your gut), which is made up of your stomach, pancreas, liver, gallbladder, small intestine, colon and rectum, is often referred to as the "second brain." It's the only organ with its own independent nervous system, comprising 100 million neurons embedded in the gut wall. Think of neurons as the messengers of your nervous system. They transmit information to nerve cells, muscles and gland cells throughout your body. This "second brain" is so robust that it can continue to function even when the primary neural connection between your gastrointestinal system and the brain (called the vagus nerve) is severed. This means that even though your brain wouldn't be able to communicate with your gut, neurons in your gut wall would still be able to transmit the information necessary for your digestive tract to function on its own. Fact No. 2: Your veins, capillaries and arteries would stretch for more than 60,000 miles if laid out flat.When your heart beats, it pumps blood through your circulatory system made up of blood vessels called arteries, capillaries and veins. These blood vessels carry blood to every part of your body: Arteries carry oxygenated blood away from the heart; veins carry blood back to the heart and capillaries connect them together. If you were to lay out the vast network of blood vessels from an average child end to end, they would stretch for over 60,000 miles! In an average adult, they would stretch for almost 100,000 miles! Your capillaries, which are your smallest blood vessels (measuring only 5 micrometers in diameter), would make up nearly 80 percent of this length. In comparison, the Earth's circumference is approximately 25,000 miles. This means the blood vessels from just one person could stretch around the Earth many times! Fact No. 3: You lose 200 million skin cells every hour, and these dead skin cells can actually decrease air pollution.Your skin grows fast. Like really fast. During a 24-hour period, you can lose up to 5 billion skin cells (that's nine zeros!) — about 200 million every hour. Your epidermis (the top layer of your skin) is continuously working to replace these lost skin cells with new ones. In fact, 95 percent of the cells in your epidermis work to make these new skin cells. The other 5 percent produce melanin, which gives skin its color. According to the American Chemical Society, these dead skin cells are a significant contributor to house dust and can be beneficial. As your dead skin cells fall off and collect around your home and office, they're also taking with them skin oils such as cholesterol and squalene. Studies have shown that squalene can reduce levels of ozone – a harmful pollutant that can irritate your eyes, nose and throat and exacerbate asthma symptoms. In fact, the squalene in settled dust can reduce ozone in indoor spaces, reducing indoor pollution levels by up to 15 percent. Bonus fact: Have you ever wondered how we can lose so many skin cells each day without a break occurring in your skin's protective barrier? You're not alone! A study conducted at the Imperial College London in 2016 discovered that our skin cells can maintain a protective barrier thanks to their unique tetrakaidecahedron shape – a 14-sided, 3D shape made from six rectangular and eight hexagonal sides. This shape allows skin cells to form a tight bond with other skin cells around them. The study also discovered that epidermal cells create a protein that acts as temporary glue, binding cells together in what are called "tight junctions." The unique cell shape and this "glue" allow your skin to keep its integrity despite being thin. Fact No. 4: Your cornea is unique in that it has no blood vessels.Your cornea is the transparent part of your eye that covers the pupil (the opening at the center of your eye), the iris (the colored part of your eye) and the anterior chamber (the fluid-filled inside of your eye). The cornea's transparent nature allows light to pass onto the retina and then to the brain to process what you're seeing. What's interesting is that the only reason your cornea is transparent is that it's only one of two tissues in your body – the other being cartilage – that is entirely free of blood vessels! Scientists have known for a while the cornea is transparent and free of blood vessels, but they could never explain why until 2006. Researchers at the Harvard Department of Ophthalmology's Schepens Eye Research Institute and the Massachusetts Eye and Ear Infirmary discovered the unique phenomenon that allows the cornea to be free of blood vessels is tied to the presence of large amounts of a protein called VEGFR-3. This protein can halt angiogenesis, or the growth of blood vessels. Without these large amounts of VEGFR-3, our vision would be significantly impaired. For instance, when the cornea is clouded by injury, infection or abnormal blood vessel growth, your vision can be severely impacted, and blindness can occur. This discovery is promising for researchers looking to prevent and cure blinding eye diseases and illnesses, such as cancer, because the introduction of the protein can be used therapeutically in other tissues. Fact No. 5: Bacteria in your gut can influence your mood.We already mentioned your gut can do some pretty amazing things, but did you know it can also impact your mental health? You have an immense number of bacteria in your gut that are collectively referred to as your microbiome. This collection of bacteria can impact neural development, brain chemistry, emotional behaviors, pain perception and stress. Your gut is sterile when you're born. Over time, your GI tract will develop a diverse colony of bacterial species, which can be influenced by your genetics and the bacteria in the environment you live in. Your microbiome produces hundreds of neurochemicals that your brain uses to regulate learning, memory and even your mood! In fact, your microbiome produces approximately 95 percent of your body's serotonin, the critical hormone that stabilizes your mood, feelings of well-being and happiness. Serotonin also helps reduce depression, regulate anxiety, maintain bone health and facilitate processes such as sleeping, eating and digestion. And it's all possible thanks to your gut! Fact No. 6: Your heart rate and breathing can sync up to the music you're listening to.That's right! The music you listen to can cause physiological changes in your blood pressure, heart rate and respiration. Studies have found that changes in the cardiovascular and respiratory systems that occur when listening to music directly mirror the tempo and intensity of what you're listening to. For example, songs with crescendos (increases in volume and intensity) can lead to proportional increases in blood pressure, heart rate and breathing. In contrast, decrescendos and silent periods lead to decreases in these vitals. Researchers have also found repeated rhythms in music can cause your cardiovascular system to synchronize with the beat. These findings may lead to new therapies for stroke and other conditions. These aren't the only impacts music can have on your cardiovascular system, either. Listening to music, playing an instrument or singing have been found to enable people to exercise longer, help heart rate and blood pressure levels to return to baseline more quickly after physical exertion, improve blood vessel function by relaxing arteries, ease anxiety in heart attack survivors and help people recovering from heart surgery feel less pain and anxiety. These benefits are heightened when you're familiar with the music you're hearing, rather than listening to songs you don't know. Fact No. 7: Your brain shrinks during pregnancy.This fact gives an entirely new meaning to the term "pregnancy brain." A 2017 study published in the journal Nature Neuroscience revealed pregnant women experience reductions in cortical thickness and surface area in sections of the brain called grey matter. This loss of grey matter primarily occurs in the cerebral cortex, specifically in regions that influence social cognition, where we process people's feelings and nonverbal signals. Rather than having a negative effect, this loss of volume improves the brain's ability to process social situations more efficiently, especially when interpreting babies' needs and emotions. The study found the brain goes through these changes, which are thought to be evolutionary, during pregnancy to enhance emotion and facial recognition, promote mother-infant bonding, facilitate a mother's ability to recognize the needs of her child and more quickly process social stimuli that may pose a potential threat to her child. These grey matter reductions were seen to have endured for at least two years post-pregnancy, offering the first evidence that pregnancy leaves long-lasting changes in a women's brain.
Subscribe to the INTEGRIS On Your Health blogSubscribe for regular emails full of useful and interesting Oklahoma-centric health and wellness info, from the doctors and health experts at INTEGRIS. Share this page |
| You are subscribed to email updates from "respiratory system disorders,respiratory system facts,respiratory tract infection" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |

Comments
Post a Comment